Navigating such a big and important surgery can feel overwhelming. There are many people and resources available to help get you through surgery and, ultimately, get you living a more comfortable and healthy life. You can also prepare yourself by reading and learning as much as you can before heading into surgery. Learn more about the HVAD surgery journey:
-
Preparing
for Surgery -
After Surgery
-
Recovery Self Care
-
Daily Life
and Safety -
Discharge
Preparing for Surgery
What should you expect before VAD surgery? Watch the video below to understand what to expect on your HVAD™ System surgery day.

Download PDF

Download PDF
Throughout your journey, your care team will support you, guide you, and answer any questions or concerns you have. Everyone’s journey will look a little different. Use the HVAD™ System Patient Journey map to get a feel for what lies ahead. This map will also help you understand when you should be reading and learning about different phases of the journey.
There are some important things to consider before starting on your journey. Use these resources to learn more about what lies ahead.
Your Surgery Day
How is the HVAD implanted in the chest?
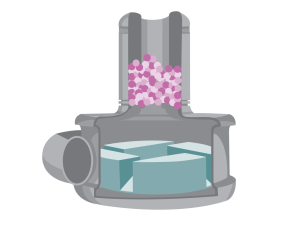
The surgery can take an entire day. The surgeon performs a sternotomy, which involves opening your chest and implanting the HVAD™ System device into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation.
Explore this interactive to learn more about the surgery.
After Surgery
What should you expect after VAD surgery? Watch the video below to understand what to expect after surgery with a HVAD™ System.
After the operation, you will recover in the ICU. You will have a breathing tube that’s connected to a ventilator (breathing machine) and you will be connected to many lines, tubes, and medical equipment.

This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal.
As with any surgery, you will probably feel some pain afterwards. Learn more about what to expect in the interactive below:

The Cardiac Step-Down Unit
The Cardiac Step-Down Unit, or cardiac floor, is where you may be transferred after the ICU. This floor is for patients who are not as critically ill but still need to be in the hospital. On the cardiac floor, you will focus on getting stronger. During this time, education will become even more important so that you can be discharged from the hospital. However, in some cases, this is not possible. Your care team will discuss this with you.
Recovery Self Care
When you have a VAD there is a lot for you and your caregivers to learn.
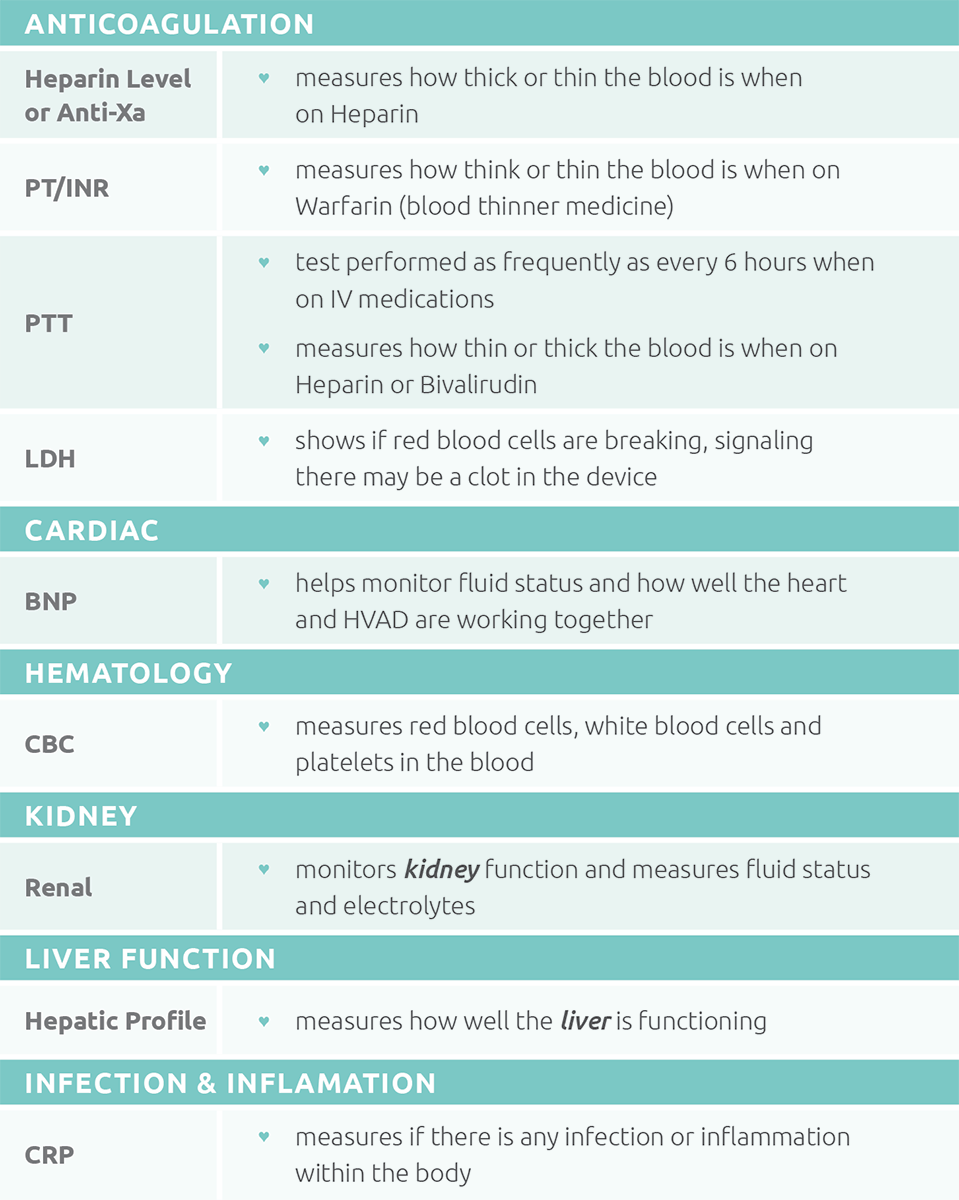
What labs could you need?
You will have laboratory testing (labs or bloodwork) done at various scheduled times or whenever your care team feels they need to follow you closer. These labs tell your care team how well your body is functioning with the new device.
Click on the image to view a list of possible requested labs.
What tests could you need?
Testing will become part of normal life. Testing will be done at scheduled times and whenever your team feels like you may need closer surveillance.
- IMPORTANT: Once you have a VAD, DO NOT have an MRI test. An MRI uses strong magnets that attract metal objects and would damage your VAD.
Common tests include:
- CT Scan: If the VAD is acting unusual or your LDH is high, your team may order a CT scan of your heart to check for a clot in the device. A CT of your head may be done if there is a concern for stroke.
- Echocardiogram: An “Echo” is an ultrasound that uses nonradioactive, high-frequency sound waves to view your heart. An Echo is a non-invasive test and helps the care team to diagnose any heart or VAD problems.
- Exercise Testing: To determine how well you are doing on the VAD, your team may order an exercise test. The exercise test may be done on a stationary bike, a treadmill, or they may have you do a 6 minute walk.
- Ramp Study: A Ramp Study is done to determine the best RPM setting for you. The team will watch how your heart looks as they change the speed of the device.
What medicines could you take?
In the hospital, medicine will be given through an IV. Your care team will change those medicines to be given by mouth when preparing for discharge. It’s important the medicines are taken at the same time every day. By the time you are ready to go home, medicines will likely be taken twice a day. Use a pill box to keep your medicines organized. Inform your care team if you take any additional medicines NOT prescribed by them. Learn more about medicines through the interactive below. Blood Thinning Medicines When you are on a VAD, you will always be on blood thinner (anticoagulation) medicines. Your care team will increase and decrease the medicines based on your lab results.Aspirin
You will take aspirin to prevent platelets from sticking together and forming a clot in your VAD.
Warfarin (Coumadin)
Warfarin is the most important medicine you will take, but it can be difficult to get your dose (the amount you take) correct. The dose needed will go up and down frequently depending on your INR. Warfarin is what makes your INR (blood levels for anticoagulation or how thick or thin your blood is) increase. In can be tricky because it interacts with lots of different medicines and foods. Your INR can change dramatically with your diet. Warfarin blocks the ability for the body to activate Vitamin K, which helps your body produce blood clots. Green leafy vegetables are rich in vitamin K. Eating lots of these types of foods can decrease your INR or make your blood thicker. It is important to have a consistent diet that includes serving of foods that contain similar amounts of vitamin K each week.

Causes for High INR (thin blood):
- New medicines
- Prolonged vomiting/diarrhea*
- Prolonged inability to eat*
- An increase in alcohol consumption
- A decreased intake of food or drink containing vitamin K
Causes for Low INR (thick blood):
- Missed doses of warfarin
- An increased intake of food or drink containing vitamin K
- Large increase in exercise
Learn more about warfarin (Coumadin) in the Exploring Medicine Treatment Options module and learn more about anticoagulation through the interactive below.
High Blood Pressure Medicines
At times, with a VAD you may have high blood pressure and require medicines to keep the VAD pumping well and can decrease your risk of stroke.
Antibiotics
Antibiotics are given in the operating room and ICU to prevent infection. They are also given if your driveline gets infected. Antibiotics can make your INR high or low. Immediately notify your care team if you start taking an antibiotic.
Stomach Ulcer & Acid Reflux Medicines
Medicines to prevent “heartburn” are used to decrease the acid in the stomach. This may help with decreasing any stomach discomfort you may have.
Diuretics (medicines to remove extra body water)
Diuretics were important when you were in heart failure. When you are on a VAD you should need less, but you still may need a small amount to get the fluids in your body just right.
What complications could occur?
Most of the following complications are rare and your care team will be with there to help keep you safe.
Bleeding
When on blood thinners, you are always at risk of bleeding. You may experience bleeding from your gums when brushing your teeth and your cuts may bleed more than normal. Girls may experience heavier bleeding during menstrual periods and may need to seek additional treatment. If you are involved in a traumatic accident, such as a car accident, it can be harder to stop the bleeding.
Nose Bleeds
To prevent nose bleeds, use petroleum jelly or saline nose spray in your nasal passages during cold, dry weather. Do not pick your nose as this may start a nosebleed. If you have a nose bleed:
- Stay calm. Look forward. Do not tilt your head back.
- Hold pressure at the bridge of your nose for 10 minutes without letting go.
- If pressure doesn’t stop the bleeding, your care team may advise you to use Afrin® or saline nasal spray.
- Let your care team know if you can’t stop the bleeding, or if you have frequent nose bleeds.
Gastrointestinal (GI) Bleeds
Learn more about the risks and signs of bleeding in your belly in the interactive below.
Stroke
With all VADs there is a risk of stroke, which is caused by bleeding or a blood clot in your brain. Both may cause injury to your brain. Your care team manages your medicines carefully to prevent strokes, however sometimes strokes may occur. Notify your care team or call 911 if you have any of the following symptoms:
- Headaches that are different than usual
- Numbness and/or tingling on one side of the body
- Weakness on one side of the body
- Losing feeling and/or movement in the legs or arms
- Slurring words or trouble when talking
- Facial expressions and movements don’t match (or mirror) on each side of the face
- Pupil (the dark circle in the middle of the eye) sizes don’t match

Download PDF
Hemolysis
Red blood cells help carry oxygen to your tissues and organs. When red blood cells get broken down, this is called hemolysis. Hemolysis may occur for multiple reasons, the most concerning being a mechanical problem with the VAD. Notify your care team if you have any of the following symptoms:
- Pink, red, cola, or tea colored urine
- Increased pump power/flow that is out of your range
- Decreased pump power that is out of your range
Learn more about what to look out for in the interactive below:
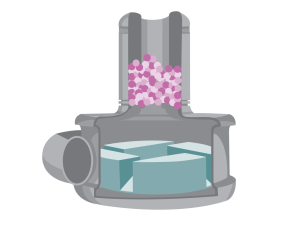
Pump Clots
Rarely will the VAD develop a clot inside of it and not work properly. If this happens, and changes to your blood thinner medicine doesn’t fix the problem, you may need to get a new VAD.
What should you know about your blood pressure?
Keeping your blood pressure in a healthy range is very important. Your care team will determine a target blood pressure goal and adjust medicines to meet it. Blood pressure can be monitored using a blood pressure cuff and/ or a Doppler. This depends on if you can feel a pulse. If you go to an outside hospital you may need to tell them the best way to take your blood pressure.
Learn more in the interactive below about how your care team will help you stay at a healthy blood pressure.
How do you care for your driveline site?
Caring for your driveline will help you avoid getting an infection. Germs that collect at the driveline site could travel to the heart if left untreated. Frequent movement of the driveline can cause damage above and underneath the skin and increase the risk of infection. Using anchors to keep the driveline in place is important to keep the driveline site healthy.
If you notice any changes in your driveline or if your driveline gets pulled, tell your care team right away so it can be treated quickly. Signs and symptoms of a driveline infection include:
- Redness
- Pain or tenderness
- Drainage (new or increased)
- Swelling and warmth
Learn more about what to look out for through the infection interactive below
Dressing Changes
Your driveline site will need to have dressing changes using a sterile technique. Everyone should use sterile gloves and wear masks during dressing changes. How often you change your dressings will be determined by your care team.
Learn more about how to properly clean and take care of your driveline in the interactive below.
What should you be eating and drinking?
Once you have your VAD, you must stay on a stable diet. Eating a consistent healthy diet will help you heal and get stronger.
Fluid balance is very important to maintain VAD flow. Dehydration from not drinking enough or increased fluid losses (vomiting, diarrhea, sweating) will lead to low VAD blood flow.
- lightheadedness, tiredness, falls
- alarms from your VAD
- swollen face, hands or legs
- poor appetite
- shortness of breath

How are you feeling?
For some patients, having a VAD and needing lots of medical care can be hard. Many patients that have VAD surgery notice an improvement in symptoms while they are in the hospital, but it can take months for you to get stronger and recover. As you recover, you or your caregiver may feel sad, worried, or even angry at times. This is normal. Be honest about how you’re feeling and talk with your care team if you have these feelings or any changes in behavior. Taking care of your emotional and mental health is a very important part of your care. Your care team will be able to connect you with the right support services.
Daily Life and Safety
There are many things to learn about your new VAD. Watch the video below for tips to keep you safe.
What to pack in your VAD “Go Bag”?
You must always have back up equipment with you in case something happens to one of your VAD components. The following items should be with you at all times:
- Emergency VAD contact information
- Extra batteries
- Extra controller
- Medicines to take while you are gone
- Water bottle

What to know about travel?
As a precaution, always carry your VAD emergency information with you.

Driving Precautions
Every state has different rules about driving with a VAD. If you are a licensed driver, use caution within the first 90 days after surgery because you may still be taking medication that may affect your concentration. Some medications will cause side effects that you won’t have adjusted to yet. When you start driving again, take short supervised trips to get used to driving with the new equipment. If you feel dizzy, short of breath, or have blurred vision, pull over to the side of the road immediately and call for help.
Long Distance and Air Travel
You will be able to travel, even on a plane, but it takes some extra planning with your care team to make sure you’re safe. You will need a travel plan and an emergency action plan for long-distance trips. Your care team will make this plan and contact other ACTION hospitals to discuss your care. When traveling by plane, you will NOT go through standard security. You will need to tell the airline agents you have a medical device and they will take you through a separate security lane.
What should you know about going back to school or work?

It will vary from hospital to hospital, but once your care team decides it’s safe for you to return home and go to school or work, or perform your normal activities, multiple steps will occur to ensure your safety. When you do leave the hospital, make sure to:
- Have a trained person available to help with alarms and emergencies
- Notify the local EMS department (fire station, police, etc.)
- Have backup batteries, a backup controller, and any additional information your team gives you to prepare for leaving the hospital
Is exercise right for you?
 Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.
If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily.
Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.
If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily. What do you do when you get a cold?
When you have a VAD, you can still get common colds or other infections unrelated to the VAD. It’s important to have a flu shot every year. And, you should always let your care team know if you are sick. They may direct you to your primary care doctor or have you come into the VAD clinic. Learn about VAD-related infections and inflammation in the interactive below.What over-the-counter medicines can you take?
When you’re on a VAD, you will sometimes have pain, especially after your surgery.- You CAN’T take NSAIDS (Motrin, Advil, Ibuprofen) because it will change the way your blood clots.
- You CAN take Tylenol for pain.
Additional Safety Tips:
- Prevent exposure to static electricity. Use dryer sheets when doing laundry, wear rubber sole shoes/slippers indoors, and be careful on outdoor slides.
- Protect your controller and batteries when it is raining outside or when around a large amount of water.
- Always wear a seatbelt in the car.
- Never disconnect your driveline. Your pump will stop. Never disconnect from both power sources.
- Wash your hands before doing a dressing change.
- Always bring your backup equipment when leaving the house. Check the battery charge level before connecting to batteries.
- If there is a power outage, switch to battery power. Notify your care team if the power is out for more than 24 hours.
- For bleeding cuts, firmly press on the cut for 5–10 minutes, or until the bleeding stops. Call your care team if the bleeding does not stop.
Discharge
 As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged
As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged
When should you call your care team?

- Change in pump parameters, equipment issues, and alarms
- Blood pressure outside your goal ranges
- Changes in your diet
- New medicines
- Pain or bleeding
- Fever
- Changes to driveline sites
- Red, pink, cola, or tea colored urine
- Changes in your mood or anything else you feel uneasy about
Learn more about how to get ready to leave the hospital in the interactive below:
What should I tell my local emergency services? (Medical Services/Fire/Utilities)
 Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
- IMPORTANT: In the event that an emergency occurs, please tell the emergency medical services team you have a HVAD™ System.
Emergency Medical Safety Card
Always carry your medical safety card with you in case of an emergency. If you don’t have a medical safety card, download and fill out the ACTION VAD Emergency Medical Safety Card below.
Preparing for Surgery
What should you expect before VAD surgery? Watch the video below to understand what to expect on your HVAD™ System surgery day.

Download PDF

Download PDF
Throughout your journey, your care team will support you, guide you, and answer any questions or concerns you have. Everyone’s journey will look a little different. Use the HVAD™ System Patient Journey map to get a feel for what lies ahead. This map will also help you understand when you should be reading and learning about different phases of the journey.
There are some important things to consider before starting on your journey. Use these resources to learn more about what lies ahead.
Your Surgery Day
How is the HVAD implanted in the chest?
The surgery can take an entire day. The surgeon performs a sternotomy, which involves opening your chest and implanting the HVAD™ System device into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation.
Explore this interactive to learn more about the surgery.
After Surgery
What should you expect after VAD surgery? Watch the video below to understand what to expect after surgery with a HVAD™ System.
After the operation, you will recover in the ICU. You will have a breathing tube that’s connected to a ventilator (breathing machine) and you will be connected to many lines, tubes, and medical equipment.

This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal.
As with any surgery, you will probably feel some pain afterwards. Learn more about what to expect in the interactive below:

The Cardiac Step-Down Unit
The Cardiac Step-Down Unit, or cardiac floor, is where you may be transferred after the ICU. This floor is for patients who are not as critically ill but still need to be in the hospital. On the cardiac floor, you will focus on getting stronger. During this time, education will become even more important so that you can be discharged from the hospital. However, in some cases, this is not possible. Your care team will discuss this with you.
Recovery Self Care
When you have a VAD there is a lot for you and your caregivers to learn.
What labs could you need?
You will have laboratory testing (labs or bloodwork) done at various scheduled times or whenever your care team feels they need to follow you closer. These labs tell your care team how well your body is functioning with the new device.
Click on the image to view a list of possible requested labs.
What tests could you need?
Testing will become part of normal life. Testing will be done at scheduled times and whenever your team feels like you may need closer surveillance.
- IMPORTANT: Once you have a VAD, DO NOT have an MRI test. An MRI uses strong magnets that attract metal objects and would damage your VAD.
Common tests include:
- CT Scan: If the VAD is acting unusual or your LDH is high, your team may order a CT scan of your heart to check for a clot in the device. A CT of your head may be done if there is a concern for stroke.
- Echocardiogram: An “Echo” is an ultrasound that uses nonradioactive, high-frequency sound waves to view your heart. An Echo is a non-invasive test and helps the care team to diagnose any heart or VAD problems.
- Exercise Testing: To determine how well you are doing on the VAD, your team may order an exercise test. The exercise test may be done on a stationary bike, a treadmill, or they may have you do a 6 minute walk.
- Ramp Study: A Ramp Study is done to determine the best RPM setting for you. The team will watch how your heart looks as they change the speed of the device.
What medicines could you take?
In the hospital, medicine will be given through an IV. Your care team will change those medicines to be given by mouth when preparing for discharge. It’s important the medicines are taken at the same time every day. By the time you are ready to go home, medicines will likely be taken twice a day. Use a pill box to keep your medicines organized. Inform your care team if you take any additional medicines NOT prescribed by them. Learn more about medicines through the interactive below. Blood Thinning Medicines When you are on a VAD, you will always be on blood thinner (anticoagulation) medicines. Your care team will increase and decrease the medicines based on your lab results.Aspirin
You will take aspirin to prevent platelets from sticking together and forming a clot in your VAD.
Warfarin (Coumadin)
Warfarin is the most important medicine you will take, but it can be difficult to get your dose (the amount you take) correct. The dose needed will go up and down frequently depending on your INR. Warfarin is what makes your INR (blood levels for anticoagulation or how thick or thin your blood is) increase. In can be tricky because it interacts with lots of different medicines and foods. Your INR can change dramatically with your diet. Warfarin blocks the ability for the body to activate Vitamin K, which helps your body produce blood clots. Green leafy vegetables are rich in vitamin K. Eating lots of these types of foods can decrease your INR or make your blood thicker. It is important to have a consistent diet that includes serving of foods that contain similar amounts of vitamin K each week.

Causes for High INR (thin blood):
- New medicines
- Prolonged vomiting/diarrhea*
- Prolonged inability to eat*
- An increase in alcohol consumption
- A decreased intake of food or drink containing vitamin K
Causes for Low INR (thick blood):
- Missed doses of warfarin
- An increased intake of food or drink containing vitamin K
- Large increase in exercise
Learn more about warfarin (Coumadin) in the Exploring Medicine Treatment Options module and learn more about anticoagulation through the interactive below.
High Blood Pressure Medicines
At times, with a VAD you may have high blood pressure and require medicines to keep the VAD pumping well and can decrease your risk of stroke.
Antibiotics
Antibiotics are given in the operating room and ICU to prevent infection. They are also given if your driveline gets infected. Antibiotics can make your INR high or low. Immediately notify your care team if you start taking an antibiotic.
Stomach Ulcer & Acid Reflux Medicines
Medicines to prevent “heartburn” are used to decrease the acid in the stomach. This may help with decreasing any stomach discomfort you may have.
Diuretics (medicines to remove extra body water)
Diuretics were important when you were in heart failure. When you are on a VAD you should need less, but you still may need a small amount to get the fluids in your body just right.
What complications could occur?
Most of the following complications are rare and your care team will be with there to help keep you safe.
Bleeding
When on blood thinners, you are always at risk of bleeding. You may experience bleeding from your gums when brushing your teeth and your cuts may bleed more than normal. Girls may experience heavier bleeding during menstrual periods and may need to seek additional treatment. If you are involved in a traumatic accident, such as a car accident, it can be harder to stop the bleeding.
Nose Bleeds
To prevent nose bleeds, use petroleum jelly or saline nose spray in your nasal passages during cold, dry weather. Do not pick your nose as this may start a nosebleed. If you have a nose bleed:
- Stay calm. Look forward. Do not tilt your head back.
- Hold pressure at the bridge of your nose for 10 minutes without letting go.
- If pressure doesn’t stop the bleeding, your care team may advise you to use Afrin® or saline nasal spray.
- Let your care team know if you can’t stop the bleeding, or if you have frequent nose bleeds.
Gastrointestinal (GI) Bleeds
Learn more about the risks and signs of bleeding in your belly in the interactive below.
Stroke
With all VADs there is a risk of stroke, which is caused by bleeding or a blood clot in your brain. Both may cause injury to your brain. Your care team manages your medicines carefully to prevent strokes, however sometimes strokes may occur. Notify your care team or call 911 if you have any of the following symptoms:
- Headaches that are different than usual
- Numbness and/or tingling on one side of the body
- Weakness on one side of the body
- Losing feeling and/or movement in the legs or arms
- Slurring words or trouble when talking
- Facial expressions and movements don’t match (or mirror) on each side of the face
- Pupil (the dark circle in the middle of the eye) sizes don’t match

Download PDF
Hemolysis
Red blood cells help carry oxygen to your tissues and organs. When red blood cells get broken down, this is called hemolysis. Hemolysis may occur for multiple reasons, the most concerning being a mechanical problem with the VAD. Notify your care team if you have any of the following symptoms:
- Pink, red, cola, or tea colored urine
- Increased pump power/flow that is out of your range
- Decreased pump power that is out of your range
Learn more about what to look out for in the interactive below:
Pump Clots
Rarely will the VAD develop a clot inside of it and not work properly. If this happens, and changes to your blood thinner medicine doesn’t fix the problem, you may need to get a new VAD.
What should you know about your blood pressure?
Keeping your blood pressure in a healthy range is very important. Your care team will determine a target blood pressure goal and adjust medicines to meet it. Blood pressure can be monitored using a blood pressure cuff and/ or a Doppler. This depends on if you can feel a pulse. If you go to an outside hospital you may need to tell them the best way to take your blood pressure.
Learn more in the interactive below about how your care team will help you stay at a healthy blood pressure.
How do you care for your driveline site?
Caring for your driveline will help you avoid getting an infection. Germs that collect at the driveline site could travel to the heart if left untreated. Frequent movement of the driveline can cause damage above and underneath the skin and increase the risk of infection. Using anchors to keep the driveline in place is important to keep the driveline site healthy.
If you notice any changes in your driveline or if your driveline gets pulled, tell your care team right away so it can be treated quickly. Signs and symptoms of a driveline infection include:
- Redness
- Pain or tenderness
- Drainage (new or increased)
- Swelling and warmth
Learn more about what to look out for through the infection interactive below
Dressing Changes
Your driveline site will need to have dressing changes using a sterile technique. Everyone should use sterile gloves and wear masks during dressing changes. How often you change your dressings will be determined by your care team.
Learn more about how to properly clean and take care of your driveline in the interactive below.
What should you be eating and drinking?
Once you have your VAD, you must stay on a stable diet. Eating a consistent healthy diet will help you heal and get stronger.
Fluid balance is very important to maintain VAD flow. Dehydration from not drinking enough or increased fluid losses (vomiting, diarrhea, sweating) will lead to low VAD blood flow.
- lightheadedness, tiredness, falls
- alarms from your VAD
- swollen face, hands or legs
- poor appetite
- shortness of breath

How are you feeling?
For some patients, having a VAD and needing lots of medical care can be hard. Many patients that have VAD surgery notice an improvement in symptoms while they are in the hospital, but it can take months for you to get stronger and recover. As you recover, you or your caregiver may feel sad, worried, or even angry at times. This is normal. Be honest about how you’re feeling and talk with your care team if you have these feelings or any changes in behavior. Taking care of your emotional and mental health is a very important part of your care. Your care team will be able to connect you with the right support services.
Daily Life and Safety
There are many things to learn about your new VAD. Watch the video below for tips to keep you safe.
What to pack in your VAD “Go Bag”?
You must always have back up equipment with you in case something happens to one of your VAD components. The following items should be with you at all times:
- Emergency VAD contact information
- Extra batteries
- Extra controller
- Medicines to take while you are gone
- Water bottle

What to know about travel?
As a precaution, always carry your VAD emergency information with you.

Driving Precautions
Every state has different rules about driving with a VAD. If you are a licensed driver, use caution within the first 90 days after surgery because you may still be taking medication that may affect your concentration. Some medications will cause side effects that you won’t have adjusted to yet. When you start driving again, take short supervised trips to get used to driving with the new equipment. If you feel dizzy, short of breath, or have blurred vision, pull over to the side of the road immediately and call for help.
Long Distance and Air Travel
You will be able to travel, even on a plane, but it takes some extra planning with your care team to make sure you’re safe. You will need a travel plan and an emergency action plan for long-distance trips. Your care team will make this plan and contact other ACTION hospitals to discuss your care. When traveling by plane, you will NOT go through standard security. You will need to tell the airline agents you have a medical device and they will take you through a separate security lane.
What should you know about going back to school or work?

It will vary from hospital to hospital, but once your care team decides it’s safe for you to return home and go to school or work, or perform your normal activities, multiple steps will occur to ensure your safety. When you do leave the hospital, make sure to:
- Have a trained person available to help with alarms and emergencies
- Notify the local EMS department (fire station, police, etc.)
- Have backup batteries, a backup controller, and any additional information your team gives you to prepare for leaving the hospital
Is exercise right for you?
 Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.
If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily.
Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.
If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily. What do you do when you get a cold?
When you have a VAD, you can still get common colds or other infections unrelated to the VAD. It’s important to have a flu shot every year. And, you should always let your care team know if you are sick. They may direct you to your primary care doctor or have you come into the VAD clinic. Learn about VAD-related infections and inflammation in the interactive below.What over-the-counter medicines can you take?
When you’re on a VAD, you will sometimes have pain, especially after your surgery.- You CAN’T take NSAIDS (Motrin, Advil, Ibuprofen) because it will change the way your blood clots.
- You CAN take Tylenol for pain.
Additional Safety Tips:
- Prevent exposure to static electricity. Use dryer sheets when doing laundry, wear rubber sole shoes/slippers indoors, and be careful on outdoor slides.
- Protect your controller and batteries when it is raining outside or when around a large amount of water.
- Always wear a seatbelt in the car.
- Never disconnect your driveline. Your pump will stop. Never disconnect from both power sources.
- Wash your hands before doing a dressing change.
- Always bring your backup equipment when leaving the house. Check the battery charge level before connecting to batteries.
- If there is a power outage, switch to battery power. Notify your care team if the power is out for more than 24 hours.
- For bleeding cuts, firmly press on the cut for 5–10 minutes, or until the bleeding stops. Call your care team if the bleeding does not stop.
Discharge
 As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged
As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged
When should you call your care team?

- Change in pump parameters, equipment issues, and alarms
- Blood pressure outside your goal ranges
- Changes in your diet
- New medicines
- Pain or bleeding
- Fever
- Changes to driveline sites
- Red, pink, cola, or tea colored urine
- Changes in your mood or anything else you feel uneasy about
Learn more about how to get ready to leave the hospital in the interactive below:
What should I tell my local emergency services? (Medical Services/Fire/Utilities)
 Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
- IMPORTANT: In the event that an emergency occurs, please tell the emergency medical services team you have a HVAD™ System.
Emergency Medical Safety Card
Always carry your medical safety card with you in case of an emergency. If you don’t have a medical safety card, download and fill out the ACTION VAD Emergency Medical Safety Card below.