Navigating such a big and important surgery can feel overwhelming. There are many people and resources available to help you get through your surgery journey and ultimately get you living a more comfortable and healthy life. You can also prepare by reading and learning as much as you can before heading into surgery.
-
Preparing for Surgery
-
After Surgery
-
Recovery Self Care
-
Discharge
Preparing for Surgery

Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.
Before your surgery, doctors called anesthesiologists will visit you. They are responsible for keeping you asleep during surgery. You will not feel any pain while you are asleep. All you will remember is traveling down to the operating room.
Your Surgery Day
How is the VAD implanted in the chest?
The surgery can take all day. The surgeon performs a sternotomy, which involves opening the chest, cutting away the diseased ventricles and valves, and connecting the TAH-t to the upper heart chambers (or atria). This will leave a scar on the chest. A heart and lung bypass machine is required to circulate your blood during the surgery.
After Surgery

When you wake up from surgery, you will be in the Intensive Care Unit (ICU).
Surgery, and the medications that you were given to keep you asleep, will make you very weak and sleepy. You will have a breathing tube that’s connected to a ventilator (breathing machine) and you will be connected to many lines, tubes, and medical equipment.
This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal.
As with any surgery, you will probably feel some pain afterwards. Learn more in the interactive below about what to expect.
Once your care team thinks you’re strong enough to be more awake and breathe on your own, your medicines keeping you sleepy will be turned off. Your breathing tube will be removed, and you will be given oxygen using a nasal cannula or mask.
As time goes on, you’ll be able to drink clear fluids like water and apple juice. When your medicines supporting your heart have been decreased, you’ll be able to eat regular food again. Your care team may decide to give you a boost of nutrition, feeding you through a special tube in your nose called a nasogastric tube.
Cardiac Step-Down Unit
The Cardiac Step-Down Unit, or cardiac floor, is where patients are transferred after the ICU. It is for patients who are not as critically ill but still need to be in the hospital. In the cardiac step-down unit, your focus will be on getting stronger. In addition, this is the time that education becomes even more important. In some cases being discharged out of the hospital may be possible. Your care team will discuss this with you.
Recovery Self Care
When you have a VAD there is a lot for you and your caregivers to learn.
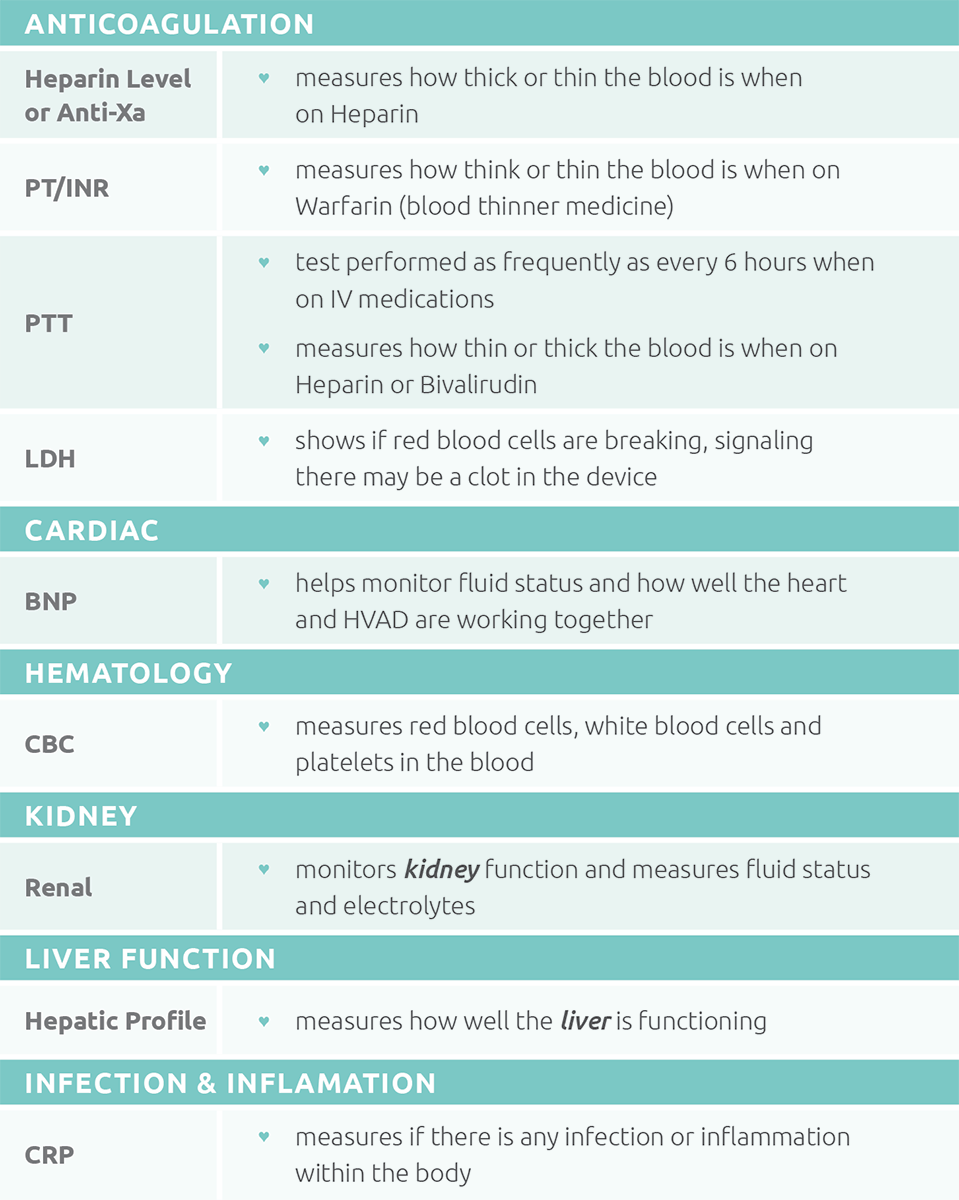
What labs could you need?
You will have laboratory testing (labs or bloodwork), done at various scheduled times or whenever your care team feels they need to follow you closer. These labs tell your doctor how well your body is functioning with the new device.
Click on the image to view a list of possible requested labs.
What tests could you need?
Testing will become part of normal life. Testing will be done at scheduled times and whenever your team feels like you may need closer surveillance.
- IMPORTANT: Once you have a SynCardia (TAH-t), DO NOT have an MRI test. An MRI uses strong magnets that attract metal objects and would damage your TAH-t.
You may, however, have an exercise test on a stationary bike, treadmill, or 6-minute walk to determine how well you are doing with the TAH-t.
What medicines could you take?
In the hospital, medicine will be given through an IV. Your care team will change those medicines to be given by mouth as you recover. It’s important the medicines are taken at the same time every day. Use a pill box to keep your medicines organized. Inform your care team if you take any additional medicines NOT prescribed by them. Learn more about medicines in the interactive below.
You will take aspirin to prevent platelets from sticking together and forming a clot in your TAH-t.
Warfarin (Coumadin)
Once your care team determines the time is right, you will take warfarin pills by mouth. Warfarin is the most important medicine you will take, but it can be difficult to get your dose (the amount you take) correct. The dose needed will go up and down frequently depending on your INR and it can take a number of days to get it right. Once your dose is correct, your IV blood thinner medicine will be turned off. Warfarin is what makes your INR (blood levels for anticoagulation or how thick or thin your blood is) increase. Below are causes for:

Causes for High INR (thin blood):
- New medicines
- Prolonged vomiting/diarrhea*
- Prolonged inability to eat*
- An increase in alcohol consumption
- A decreased intake of food or drink containing vitamin K
*Discuss with your care team
Causes for Low INR (thick blood):
- Missed doses of warfarin
- An increased intake of food or drink containing vitamin K
- Large increase in exercise
Learn more about warfarin (Coumadin) in the Exploring Medicine Treatment Options module and learn more about anticoagulation through the interactive below.
Blood Pressure Medicines
At times, on a TAH-t you may have high blood pressure and require medicines to keep the TAH-t pumping well and can decrease your risk of stroke.
Antibiotics
Antibiotics are given in the operating room and ICU to prevent infection. They are also given if your cannulae get infected. You may need antibiotics indefinitely to prevent infection. Antibiotics can make your INR high or low. Immediately notify your care team if you start taking an antibiotic.
Stomach Ulcers & Acid Reflux Medicines
Medicines to prevent “heartburn” are used to decrease the acid in the stomach. This may help with decreasing any stomach discomfort you may have.
Diuretics (medicines to remove extra body water)
Diuretics were important when you were in heart failure. When you are on a TAH-t you should need less, but you still may need a small amount to get the fluids in your body just right.
What should you know about your blood pressure?
Keeping your blood pressure in a healthy range is very important. Your care team will determine a target blood pressure goal and adjust medicines to meet it. Blood pressure can be monitored using a blood pressure cuff. Learn more in the interactive below about how your care team will help you stay at a healthy blood pressure.
Why is it important to care for your cannula site?
Caring for your cannulae will help you avoid getting an infection.
What should you be eating and drinking?
Once you have your VAD, you must stay on a stable diet. Eating a consistent healthy diet will help you heal and get stronger.
Fluid balance is very important to maintain TAH-t flow. If there is too much fluid inside the heart and body (for example, if you’re drinking much more than usual), the TAH-t may not be able to handle the extra fluid. Learn more about why it’s important to balance how much fluid you are drinking:
How are you feeling?
For some patients, having a TAH-t and needing lots of medical care can be hard. Many patients that have TAH-t surgery notice an improvement in symptoms while they are in the hospital, but it can take months for you to get stronger and recover. As you recover, you or your caregiver may feel sad, worried, or even angry at times. This is normal. Be honest about how you’re feeling and talk with your care team if you have these feelings or any changes in behavior. Taking care of your emotional and mental health is a very important part of your care. Your care team will be able to connect you with the right support services.
Discharge
 In rare cases, TAH-t patients may be discharged out of the hospital on the Freedom® Portable Driver. If your care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged.
In rare cases, TAH-t patients may be discharged out of the hospital on the Freedom® Portable Driver. If your care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged. When should you call your care team?

If you are discharged out of the hospital, you will have a detailed communication plan. The plan will include a phone number to call. Your care team will want be in contact communication with you. Things you should tell them include:
- Change in pump parameters, equipment issues, and alarms
- Blood pressure outside your goal ranges
- Changes in your diet
- New medicines
- Pain or bleeding
- Fever
- Changes to cannula sites
- Red, pink, cola, or tea colored urine
- Changes in your mood or anything else you feel uneasy about
What should I tell my local emergency services? (Medical Services/Fire/Utilities)

Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
- IMPORTANT: In the event that an emergency occurs, please tell the emergency medical services team you have a SynCardia (TAH-t). Standard CPR and code medicines may be unsafe.
Medical Safety Card
Always carry your medical safety card with you in case of an emergency. If you don’t have a medical safety card, download and fill out the ACTION VAD Emergency Medical Safety Card below.
Preparing for Surgery

Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.
Before your surgery, doctors called anesthesiologists will visit you. They are responsible for keeping you asleep during surgery. You will not feel any pain while you are asleep. All you will remember is traveling down to the operating room.
Your Surgery Day
How is the VAD implanted in the chest?
The surgery can take all day. The surgeon performs a sternotomy, which involves opening the chest, cutting away the diseased ventricles and valves, and connecting the TAH-t to the upper heart chambers (or atria). This will leave a scar on the chest. A heart and lung bypass machine is required to circulate your blood during the surgery.
After Surgery

When you wake up from surgery, you will be in the Intensive Care Unit (ICU).
Surgery, and the medications that you were given to keep you asleep, will make you very weak and sleepy. You will have a breathing tube that’s connected to a ventilator (breathing machine) and you will be connected to many lines, tubes, and medical equipment.
This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal.
As with any surgery, you will probably feel some pain afterwards. Learn more in the interactive below about what to expect.
Once your care team thinks you’re strong enough to be more awake and breathe on your own, your medicines keeping you sleepy will be turned off. Your breathing tube will be removed, and you will be given oxygen using a nasal cannula or mask.
As time goes on, you’ll be able to drink clear fluids like water and apple juice. When your medicines supporting your heart have been decreased, you’ll be able to eat regular food again. Your care team may decide to give you a boost of nutrition, feeding you through a special tube in your nose called a nasogastric tube.
Cardiac Step-Down Unit
The Cardiac Step-Down Unit, or cardiac floor, is where patients are transferred after the ICU. It is for patients who are not as critically ill but still need to be in the hospital. In the cardiac step-down unit, your focus will be on getting stronger. In addition, this is the time that education becomes even more important. In some cases being discharged out of the hospital may be possible. Your care team will discuss this with you.
Recovery Self Care
When you have a VAD there is a lot for you and your caregivers to learn.
What labs could you need?
You will have laboratory testing (labs or bloodwork), done at various scheduled times or whenever your care team feels they need to follow you closer. These labs tell your doctor how well your body is functioning with the new device.
Click on the image to view a list of possible requested labs.
What tests could you need?
Testing will become part of normal life. Testing will be done at scheduled times and whenever your team feels like you may need closer surveillance.
- IMPORTANT: Once you have a SynCardia (TAH-t), DO NOT have an MRI test. An MRI uses strong magnets that attract metal objects and would damage your TAH-t.
You may, however, have an exercise test on a stationary bike, treadmill, or 6-minute walk to determine how well you are doing with the TAH-t.
What medicines could you take?
In the hospital, medicine will be given through an IV. Your care team will change those medicines to be given by mouth as you recover. It’s important the medicines are taken at the same time every day. Use a pill box to keep your medicines organized. Inform your care team if you take any additional medicines NOT prescribed by them. Learn more about medicines in the interactive below.
You will take aspirin to prevent platelets from sticking together and forming a clot in your TAH-t.
Warfarin (Coumadin)
Once your care team determines the time is right, you will take warfarin pills by mouth. Warfarin is the most important medicine you will take, but it can be difficult to get your dose (the amount you take) correct. The dose needed will go up and down frequently depending on your INR and it can take a number of days to get it right. Once your dose is correct, your IV blood thinner medicine will be turned off. Warfarin is what makes your INR (blood levels for anticoagulation or how thick or thin your blood is) increase. Below are causes for:

Causes for High INR (thin blood):
- New medicines
- Prolonged vomiting/diarrhea*
- Prolonged inability to eat*
- An increase in alcohol consumption
- A decreased intake of food or drink containing vitamin K
*Discuss with your care team
Causes for Low INR (thick blood):
- Missed doses of warfarin
- An increased intake of food or drink containing vitamin K
- Large increase in exercise
Learn more about warfarin (Coumadin) in the Exploring Medicine Treatment Options module and learn more about anticoagulation through the interactive below.
Blood Pressure Medicines
At times, on a TAH-t you may have high blood pressure and require medicines to keep the TAH-t pumping well and can decrease your risk of stroke.
Antibiotics
Antibiotics are given in the operating room and ICU to prevent infection. They are also given if your cannulae get infected. You may need antibiotics indefinitely to prevent infection. Antibiotics can make your INR high or low. Immediately notify your care team if you start taking an antibiotic.
Stomach Ulcers & Acid Reflux Medicines
Medicines to prevent “heartburn” are used to decrease the acid in the stomach. This may help with decreasing any stomach discomfort you may have.
Diuretics (medicines to remove extra body water)
Diuretics were important when you were in heart failure. When you are on a TAH-t you should need less, but you still may need a small amount to get the fluids in your body just right.
What should you know about your blood pressure?
Keeping your blood pressure in a healthy range is very important. Your care team will determine a target blood pressure goal and adjust medicines to meet it. Blood pressure can be monitored using a blood pressure cuff. Learn more in the interactive below about how your care team will help you stay at a healthy blood pressure.
Why is it important to care for your cannula site?
Caring for your cannulae will help you avoid getting an infection.
What should you be eating and drinking?
Once you have your VAD, you must stay on a stable diet. Eating a consistent healthy diet will help you heal and get stronger.
Fluid balance is very important to maintain TAH-t flow. If there is too much fluid inside the heart and body (for example, if you’re drinking much more than usual), the TAH-t may not be able to handle the extra fluid. Learn more about why it’s important to balance how much fluid you are drinking:
How are you feeling?
For some patients, having a TAH-t and needing lots of medical care can be hard. Many patients that have TAH-t surgery notice an improvement in symptoms while they are in the hospital, but it can take months for you to get stronger and recover. As you recover, you or your caregiver may feel sad, worried, or even angry at times. This is normal. Be honest about how you’re feeling and talk with your care team if you have these feelings or any changes in behavior. Taking care of your emotional and mental health is a very important part of your care. Your care team will be able to connect you with the right support services.
Discharge
 In rare cases, TAH-t patients may be discharged out of the hospital on the Freedom® Portable Driver. If your care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged.
In rare cases, TAH-t patients may be discharged out of the hospital on the Freedom® Portable Driver. If your care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged. When should you call your care team?

If you are discharged out of the hospital, you will have a detailed communication plan. The plan will include a phone number to call. Your care team will want be in contact communication with you. Things you should tell them include:
- Change in pump parameters, equipment issues, and alarms
- Blood pressure outside your goal ranges
- Changes in your diet
- New medicines
- Pain or bleeding
- Fever
- Changes to cannula sites
- Red, pink, cola, or tea colored urine
- Changes in your mood or anything else you feel uneasy about
What should I tell my local emergency services? (Medical Services/Fire/Utilities)

Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
- IMPORTANT: In the event that an emergency occurs, please tell the emergency medical services team you have a SynCardia (TAH-t). Standard CPR and code medicines may be unsafe.
Medical Safety Card
Always carry your medical safety card with you in case of an emergency. If you don’t have a medical safety card, download and fill out the ACTION VAD Emergency Medical Safety Card below.