Understanding
Your Diagnosis
Heart failure is a complicated condition and can affect people of all ages. Learn the basics about heart failure and explore the different types symptoms, risk factors, and complications.
Heart failure is a complicated condition and can affect people of all ages.
Learn the basics about heart failure and explore the different types,
symptoms, risk factors, and complications.
-
1
Overview
-
2
Causes
-
3
Testing
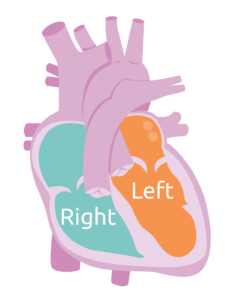
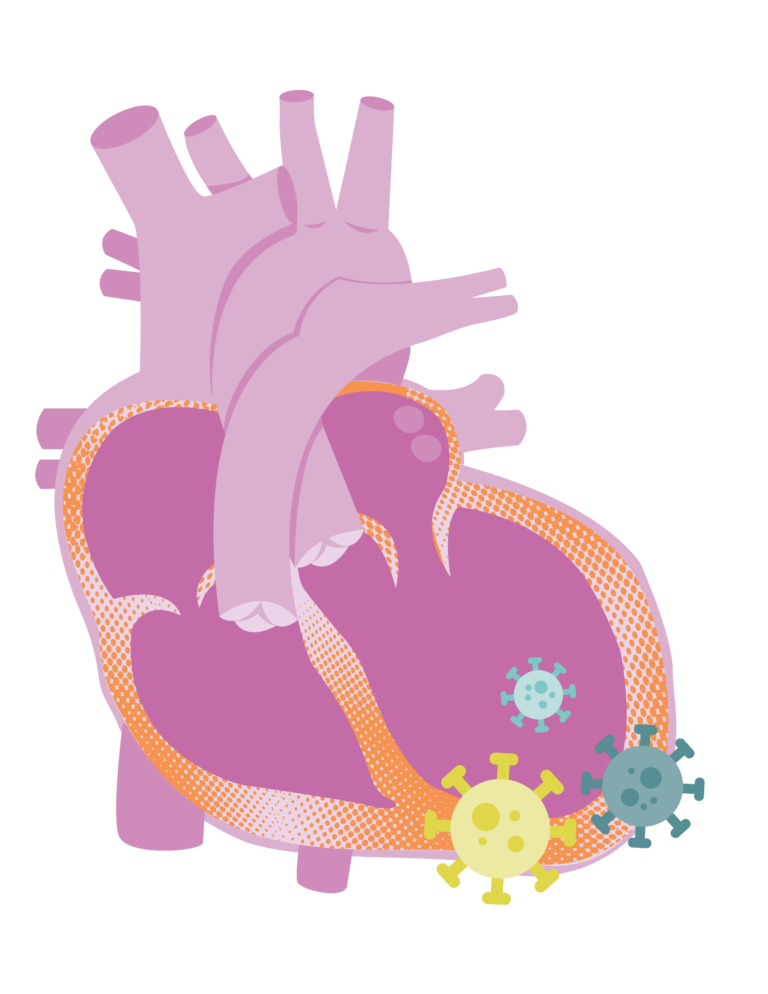
The heart is one of the most important parts of your body. But what happens when it doesn’t work like it should? This video explores what heart failure is and some of the causes. Read through our Heart A normal heart has 4 chambers: 2 atria and 2 ventricles. The right side of the heart receives deoxygenated (blue) blood from the body and pumps it to the lungs to get oxygen. The left side of the heart receives the newly oxygenated blood (red) from the lungs and pumps it to the rest of the body. The heart has two phases: contraction (systole) and relaxation (diastole). When the heart relaxes, the ventricles rest and fill up with blood sent from the atria. During contraction, the ventricles squeeze the blood to the rest of the body. Heart failure can be classified based on whether the ventricle has abnormal contraction or abnormal relaxation. Systolic Heart Failure Diastolic Heart Failure Heart failure can also involve the left ventricle (left-sided heart failure), right ventricle (right-sided heart failure), or both (biventricular). Left-sided Heart Failure Right-sided Heart Failure Biventricular Heart Failure Living with heart failure can be challenging. What does it feel like when your heart doesn’t work like it should? Life with heart failure looks different for each patient and depends on your age. Your symptoms will depend on how severe your condition is and how much of your heart is affected. Some common symptoms of heart failure include: Depending on your age and the cause of your heart failure, it’s possible that you may face some complications. Life with heart failure looks different for each patient and depends on your age. Your symptoms will depend on how severe your condition is and how much of your heart is affected. Some common symptoms of heart failure include: For more information about pediatric heart failure, see the following resource. The Children’s Cardiomyopathy Foundation developed a guidebook providing a comprehensive overview of heart failure, including signs and symptoms, diagnostic testing, medications, and advanced heart failure therapies. The resource draws on the experience and knowledge of the top pediatric heart failure specialists in the U.S. and Australia. This cross-network collaboration brought together experts in pediatric psychology, neuropsychology, cardiology, nursing, and more to address this important aspect of care for patients and families.What is Heart Failure?
Failure Success Patient and Family Education Handbook, check out An Introduction to Pediatric Heart Failure and watch the animated video below to better understand heart failure. 
Failure Success Patient & Family Education Handbook
Download
Heart Failure
Download
Normal Heart Structure
and FunctionWhat are the Different Types of Heart Failure?
If the ventricle can’t contract well enough to pump blood to all parts of the body (including your brain, muscles, and other important organs), we call it systolic heart failure. Systolic heart failure can cause you to feel unwell and weak. It can also cause your other organs to not work properly.
If the ventricle can’t relax well enough to fill properly, we call it diastolic heart failure. This can happen if your heart muscle becomes stiff or thick. Diastolic heart failure can lead to blood backing up into the lungs and cause shortness of breath. When diastolic failure is severe, your heart cannot fill up with enough blood to adequately supply your body and your important organs. Sometimes you can have both systolic and diastolic heart failure.
The left ventricle is the heart’s primary pumping chamber. With left-sided systolic failure, the left ventricle struggles to pump enough blood throughout the body. This can lead to blood building up in your lungs. As the blood backs up into your lungs, it can make it hard for you to breathe and cause you to cough, especially if you’re doing activities like exercising or playing.
Right-sided heart failure often happens as a result of left-sided heart failure. With right-sided heart failure, the right ventricle loses some of its pumping power. In other words, it becomes too weak to pump enough blood to your lungs. When the right ventricle struggles to pump, blood builds up in your liver and veins. This can cause swelling in your legs, abdomen (belly), and feet.
Biventricular heart failure is when both sides of your heart are affected. Your symptoms can be a combination of left- and right-sided failure.Symptoms
Complications
Symptoms
Complications
 Living with heart failure can be challenging. What does it feel like when your heart doesn’t work like it should?
Living with heart failure can be challenging. What does it feel like when your heart doesn’t work like it should?
 Depending on your age and the cause of your heart failure, it’s possible that you may face some complications.
Depending on your age and the cause of your heart failure, it’s possible that you may face some complications.Heart Failure Resources
Pediatric Heart Failure: A Guide for Parents and Families
Hearts & Minds: Neurodevelopment in Patients with Heart Failure & VADs
Prompted by needs and interests of our Families in ACTION (FACT) Committee, ACTION recently joined forces with a fellow Cardiac Networks United organization, the Cardiac Neurodevelopmental Outcome Collaborative to:
As we age, our hearts naturally lose some of their power to pump and fill properly. Some health conditions may cause this to happen sooner than it should. Let’s explore some of the most common causes of heart failure in children and young adults. Check out our additional resources for children and adults with congenital heart disease below. Ventricular assist devices can help adults with congenital heart disease live longer, healthier, better quality lives. Learn what factors your doctor considers when referring CHD patients for advanced heart failure consultation. Everyone’s journey will look a little different. Use this map to get a feel for what lies ahead. It will also help you understand when you should be reading and learning about different phases of the journey. Fortunately, like with other types of CHD, cardiologists and cardiac surgeons have discovered ways to allow you to survive and thrive throughout childhood with only one ventricle. If you were born with only one ventricle, you likely went through several heart surgeries early in your life and may now have a Fontan circulation. The Fontan circulation is developed when a pediatric cardiac surgeon creates a pathway for blood to return to your lungs for oxygen directly, without circulating through a ventricle. This frees up the one ventricle you have to do the hard work of pumping your blood out to your body. While the Fontan circulation can be very successful, in some cases, the one ventricle will not be able to do all the work of two ventricles and you may experience heart failure. If you have a Fontan circulation and are starting to experience heart failure, you might feel like it’s hard to catch your breath or like your heart is beating in a weird rhythm. Your skin may be more blue-tinted than usual, or you may have swelling in certain areas of your body. Occasionally, because pediatric cardiac surgeons had to make some unnatural changes in your body to create the Fontan circulation, you may develop chronic liver disease, renal insufficiency/failure, and/or problems with your intestines leading to malnutrition. If you are a patient and have a Fontan circulation and have symptoms of heart failure that can’t be controlled with medications, you may need a VAD or a transplant. VADs can help as a form of long-term therapy or they can help you survive until it’s time for your transplant. Watch now to see how ACTION is helping patients with a Fontan circulation, like Brooklyn, to live longer and healthier lives. We are actively collaborating, sharing, and innovating to figure out how best to provide life-saving therapies for Fontan patients. As someone who was born with a single ventricle heart, you have special health concerns now. This book was written by Cincinnati Children’s Fontan team for patients who had Fontan heart surgery. This Action Plan is meant to help empower patients with a Fontan, and their caregivers, to take charge of their health and understand potential warning signs that should be examined. The goal of involving a Heart Failure Specialist early is to introduce medicines or other interventions early, with the hope of reducing symptoms and improving the outcomes. For more information about Fontan, see the following resources. When you are faced with a lifelong heart condition such as congenital heart disease, it can help to connect with others who get what you’re going through. Support groups offer a way to bring people together to share information. This can also help reduce stress and worry and provide helpful education. Mended Hearts/Mended Little Hearts Sisters by Heart The Adult Congenital Heart Association (ACHA) Fortunately, like with other types of CHD, cardiologists and cardiac surgeons have discovered ways to allow you to survive and thrive throughout childhood with only one ventricle. If you were born with only one ventricle, you likely went through several heart surgeries early in your life and may now have a Fontan circulation. The Fontan circulation is developed when a pediatric cardiac surgeon creates a pathway for blood to return to your lungs for oxygen directly, without circulating through a ventricle. This frees up the one ventricle you have to do the hard work of pumping your blood out to your body. While the Fontan circulation can be very successful, in some cases, the one ventricle will not be able to do all the work of two ventricles and you may experience heart failure. If you have a Fontan circulation and are starting to experience heart failure, you might feel like it’s hard to catch your breath or like your heart is beating in a weird rhythm. Your skin may be more blue-tinted than usual, or you may have swelling in certain areas of your body. Occasionally, because pediatric cardiac surgeons had to make some unnatural changes in your body to create the Fontan circulation, you may develop chronic liver disease, renal insufficiency/failure, and/or problems with your intestines leading to malnutrition. If you are a patient and have a Fontan circulation and have symptoms of heart failure that can’t be controlled with medications, you may need a VAD or a transplant. VADs can help as a form of long-term therapy or they can help you survive until it’s time for your transplant. Watch now to see how ACTION is helping patients with a Fontan circulation, like Brooklyn, to live longer and healthier lives. We are actively collaborating, sharing, and innovating to figure out how best to provide life-saving therapies for Fontan patients. As someone who was born with a single ventricle heart, you have special health concerns now. This book was written by Cincinnati Children’s Fontan team for patients who had Fontan heart surgery. This Action Plan is meant to help empower patients with a Fontan, and their caregivers, to take charge of their health and understand potential warning signs that should be examined. The goal of involving a Heart Failure Specialist early is to introduce medicines or other interventions early, with the hope of reducing symptoms and improving the outcomes. For more information about Fontan, see the following resources. When you are faced with a lifelong heart condition such as congenital heart disease, it can help to connect with others who get what you’re going through. Support groups offer a way to bring people together to share information. This can also help reduce stress and worry and provide helpful education. Mended Hearts/Mended Little Hearts Sisters by Heart The Adult Congenital Heart Association (ACHA) The word cardiomyopathy means “heart muscle disease.” With cardiomyopathy, the heart muscle becomes damaged. This makes it hard for the heart to relax and pump blood to the rest of the body. Cardiomyopathy can be a mild disease and require little treatment. In some cases, it can be a severe disease, and these patients may need advanced therapies, such as medicines, VAD, or transplant. Different types of cardiomyopathy include: Often, the cause of cardiomyopathy is unknown, but some possible causes may include: Watch what a day in the life is like for 7-year-old HeartWare HVAD patient, Tessa. Tessa has heart failure from cardiomyopathy. Medicines did not work for Tessa, so she received a HeartWare HVAD to help her heart pump blood to her body. This device allows Tessa to wait for her heart transplant. Tessa can play, dance, and go shopping on her VAD! Cardiotoxicity is when heart damage is caused by chemicals or medicines, like chemotherapy. When you receive chemotherapy, you are given medicines to kill cancer cells in your body. Sometimes these drugs also hurt the normal cells in and around your heart. Cancer treatments can be hard on the body and may sometimes affect the heart. Your care team will watch your health closely during and after treatment to help keep your heart as healthy as possible. See this Cardiotoxicity & Cancer handout for more information. Myocarditis is when the wall of the heart muscle becomes inflamed, usually due to a viral infection. A severe case can keep your heart from working as it should. Myocarditis has many causes: For more information, see the handout below: An Introduction to Myocarditis Muscular Dystrophy (MD) is a group of diseases that make muscles become weak over time. If you have MD, it’s likely that you’ll have problems with your heart at some point in your life. In the same way that MD weakens muscles in your body, it can also weaken your heart and lead to cardiomyopathy. This is a condition in which your heart muscle struggles to pump, fill, or beat normally. For more information about Muscular Dystrophy, check out: Hypertrophic cardiomyopathy is when your heart muscle becomes too thick. This makes it harder for the heart to relax or squeeze properly. The abnormal muscle can sometimes lead to life-threatening abnormal heart rhythms or arrhythmias. This condition can go undiagnosed because you can often live with it without showing any symptoms. Cardiotoxicity is when heart damage is caused by chemicals or medicines, like chemotherapy. When you receive chemotherapy, you are given medicines to kill cancer cells in your body. Sometimes these drugs also hurt the normal cells in and around your heart. Cancer treatments can be hard on the body and may sometimes affect the heart. Your care team will watch your health closely during and after treatment to help keep your heart as healthy as possible. See this Cardiotoxicity & Cancer handout for more information. Myocarditis is when the wall of the heart muscle becomes inflamed, usually due to a viral infection. A severe case can keep your heart from working as it should. Myocarditis has many causes: For more information, see the handout below: An Introduction to Myocarditis Muscular Dystrophy (MD) is a group of diseases that make muscles become weak over time. If you have MD, it’s likely that you’ll have problems with your heart at some point in your life. In the same way that MD weakens muscles in your body, it can also weaken your heart and lead to cardiomyopathy. This is a condition in which your heart muscle struggles to pump, fill, or beat normally. For more information about Muscular Dystrophy, check out: Hypertrophic cardiomyopathy is when your heart muscle becomes too thick. This makes it harder for the heart to relax or squeeze properly. The abnormal muscle can sometimes lead to life-threatening abnormal heart rhythms or arrhythmias. This condition can go undiagnosed because you can often live with it without showing any symptoms. Beyond Cardiomyopathy and Congenital Heart Disease, there are other causes as well. When you receive a heart transplant, the new donor heart is called a “graft.” Transplanted hearts, or grafts, can develop heart failure over time. This may happen because of coronary artery disease due to chronic or recurrent rejection. Here’s what we know: Although more common in adults, children can also get the virus that causes COVID-19. Common symptoms may include fever, cough, runny nose, diarrhea, vomiting, loss of smell, or headache. Most COVID-19 infections in children are mild or get better with medical care. It’s important for all of us to help prevent the spread of COVID-19, especially among vulnerable child populations. Children and adults can reduce their risk of exposure by wearing a mask in public, social distancing, and washing hands frequently. Some children and adult patients can experience more serious problems as a result of COVID-19. These include myocarditis or multisystem inflammatory syndrome (MIS-C): When you receive a heart transplant, the new donor heart is called a “graft.” Transplanted hearts, or grafts, can develop heart failure over time. This may happen because of coronary artery disease due to chronic or recurrent rejection. Here’s what we know: Although more common in adults, children can also get the virus that causes COVID-19. Common symptoms may include fever, cough, runny nose, diarrhea, vomiting, loss of smell, or headache. Most COVID-19 infections in children are mild or get better with medical care. It’s important for all of us to help prevent the spread of COVID-19, especially among vulnerable child populations. Children and adults can reduce their risk of exposure by wearing a mask in public, social distancing, and washing hands frequently. Some children and adult patients can experience more serious problems as a result of COVID-19. These include myocarditis or multisystem inflammatory syndrome (MIS-C):
Overview
Congenital Heart Disease
Cardiomyopathy
Other Causes
Causes
Congenital Heart Disease
Overview
Overview
Congenital Heart Disease Resources
Mechanical Circulatory Support (MCS) in ACHD Patients
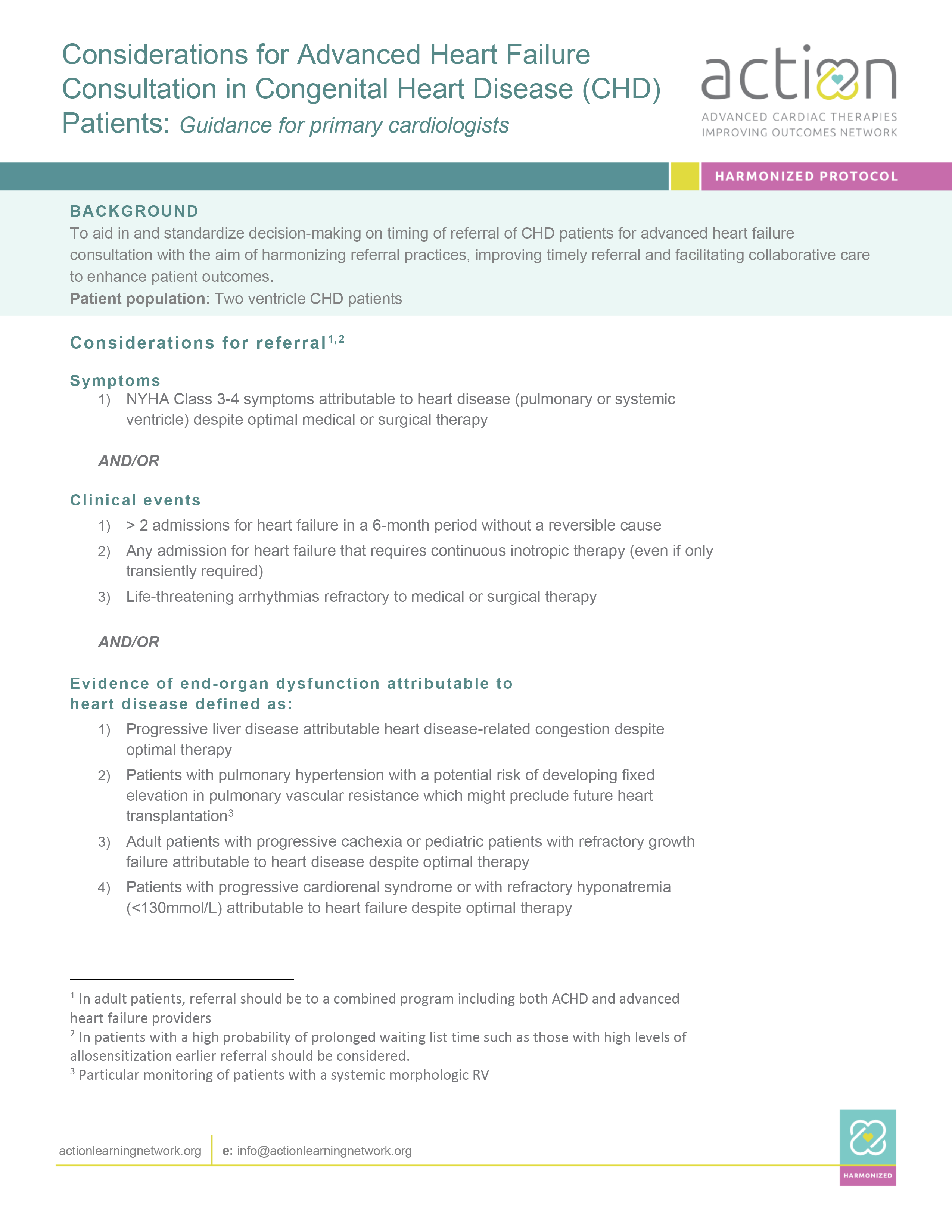
Considerations for Advanced Heart Failure Consultation in Congenital Heart Disease (CHD) Patients (CHD Referral)
HeartMate 3™ LVAD ACHD Patient Journey
Scroll down to explore specific types of congenital heart disease.
Fontan Failure
Fontan Failure

Brooklyn’s Journey
Fontan Circulation Patient Handbook
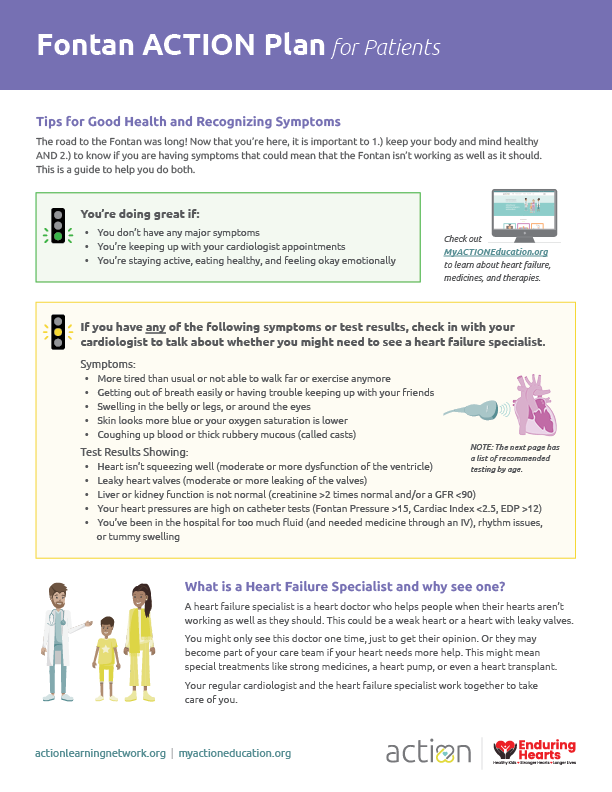
Fontan Action Plan for Patients
Fontan Resources
mendedhearts.org
sistersbyheart.org
achaheart.orgFontan Failure

Brooklyn’s Journey
Fontan Circulation Patient Handbook
Fontan Action Plan for Patients
Fontan Resources
mendedhearts.org
sistersbyheart.org
achaheart.orgCardiomyopathy
Overview
Overview
Tessa’s Journey
Scroll down to explore specific types of Cardiomyopathy.
Cardiotoxicity
Myocarditis
Muscular Dystrophy
Hypertrophic
Cardiotoxicity

Cardiotoxicity & Cancer
Myocarditis
Muscular Dystrophy
Christian & Ricky’s Stories
Christian and Ricky have Muscular Dystrophy. Both of their hearts became weakened, and heart medications did not work. They needed something to help them feel better and live longer. They each got a Ventricular Assist Device (VAD) to help their weakened hearts pump blood to their bodies. Watch as Christian and Ricky teach you about their HeartMate 3 VAD. Resources
Parent Project Muscular Dystrophy
parentprojectmd.orgHypertrophic
Cardiotoxicity

Cardiotoxicity & Cancer
Myocarditis
Muscular Dystrophy
Christian & Ricky’s Stories
Christian and Ricky have Muscular Dystrophy. Both of their hearts became weakened, and heart medications did not work. They needed something to help them feel better and live longer. They each got a Ventricular Assist Device (VAD) to help their weakened hearts pump blood to their bodies. Watch as Christian and Ricky teach you about their HeartMate 3 VAD. Resources
Parent Project Muscular Dystrophy
parentprojectmd.orgHypertrophic
Other Causes
Overview
Overview
Scroll down to explore other causes of heart failure.
Transplant
Graft FailureCOVID-19
Transplant Graft Failure
COVID-19
 To keep our children and communities safe during the COVID-19 pandemic, it is important to stay informed with updated research and medical insights.
To keep our children and communities safe during the COVID-19 pandemic, it is important to stay informed with updated research and medical insights.
Resources
COVID-19 & VADs: How to Stay Healthy in 2021
Wanna be a Health Hero?
How to Wear a Mask like a Health Hero
Transplant Graft Failure
COVID-19
 To keep our children and communities safe during the COVID-19 pandemic, it is important to stay informed with updated research and medical insights.
To keep our children and communities safe during the COVID-19 pandemic, it is important to stay informed with updated research and medical insights.
Resources
COVID-19 & VADs: How to Stay Healthy in 2021
Wanna be a Health Hero?
How to Wear a Mask like a Health Hero
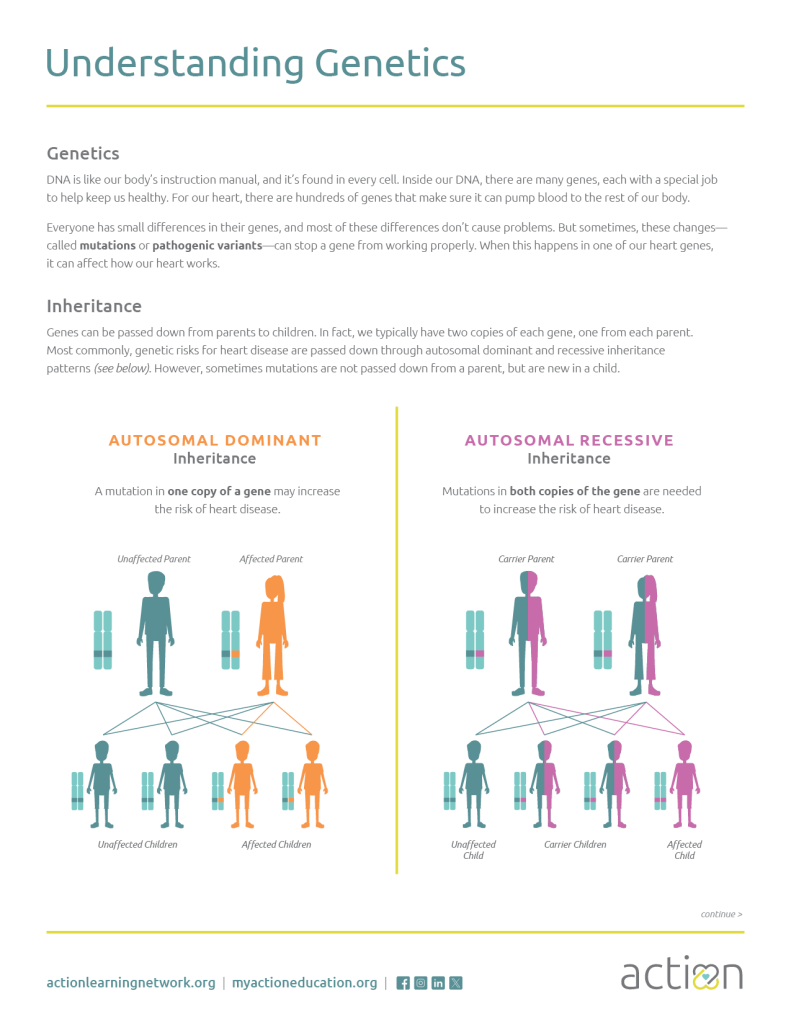
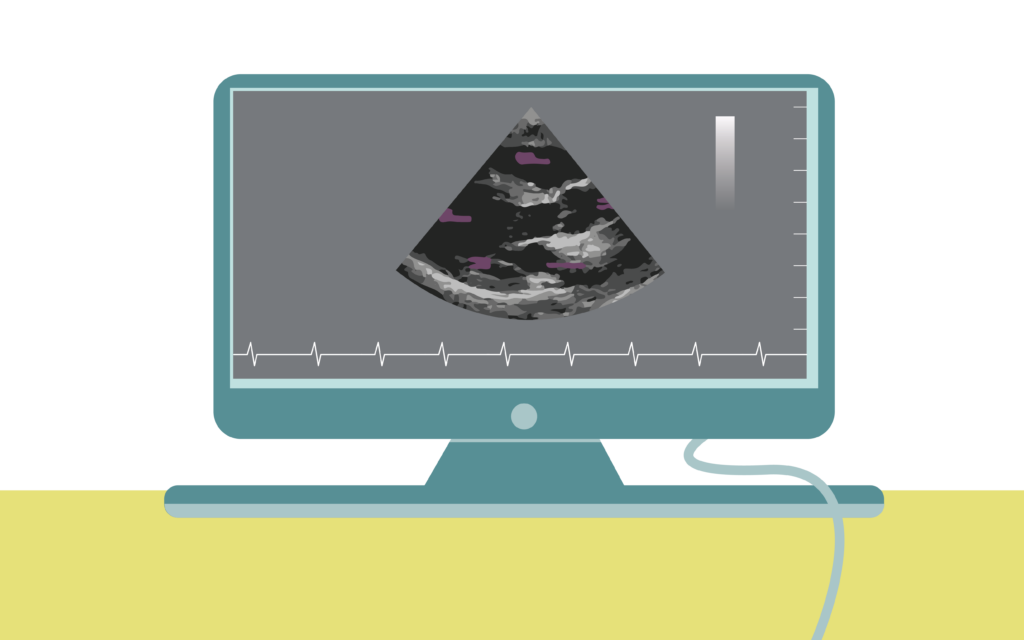
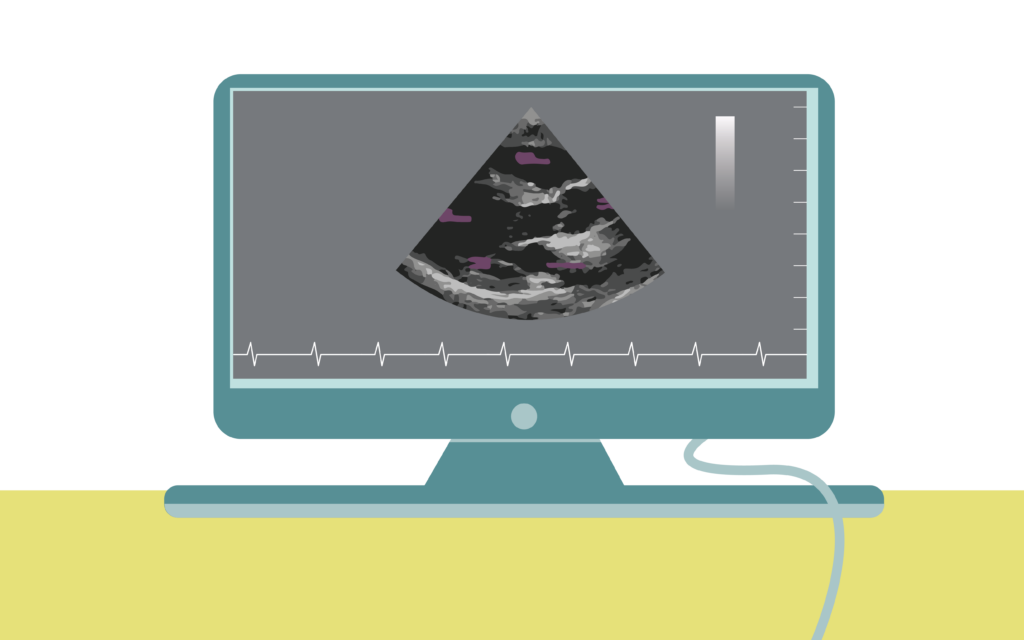
Your doctor uses several different exams and tests to understand the severity of your condition. This information helps them determine what treatment options are best for you. Genetic testing can be an important topic of discussion between providers, patients, and their families at any stage of their journey. Download this helpful tool Understanding Genetics which explains genetic testing, how genes are inherited, tips for understanding test results, and the role of Genetic Counselors as part of the care team. Heart failure is often diagnosed using an echocardiogram (or echo). An echo is an ultrasound of the heart that shows how well the four chambers are working. One of the important numbers to determine the function of the heart is called an ejection fraction (or EF%). EF is a calculation of the amount of blood pumped from the left ventricle divided by the total amount of blood that is in the heart. Normal EF is 50–70%, reduced is 40–50%, and low is <40%. The lower the percent, the more severe the heart failure. The American Heart Association explains more about Ejection Fraction in their short video. Click here to watch the video. Vitals Physical Exam The EKG shows the electrical conduction through your heart. Sometimes small changes in the EKG can be a sign that a heart is getting sicker. Once in a while, your doctor will ask you to wear a Holter monitor, which is like a portable EKG that can monitor for arrhythmias happening throughout the day. An exercise test may also be used to look for arrhythmias during exercise. It can also be helpful to check if your heart is strong enough to keep you active. There are several blood tests doctors use to diagnose heart failure. Most patients have labs drawn at scheduled times. You may have labs drawn more often if your team feels that you need closer surveillance. BNP (Brain Natriuretic Peptide) Renal Panel Liver Function Test Chest X-ray Cardiac Catheterization To see how much physical activity you can do and to check for arrhythmias during exercise, your doctor may ask you to walk up and down the hall, or exercise on a treadmill or bike. Heart failure is often diagnosed using an echocardiogram (or echo). An echo is an ultrasound of the heart that shows how well the four chambers are working. One of the important numbers to determine the function of the heart is called an ejection fraction (or EF%). EF is a calculation of the amount of blood pumped from the left ventricle divided by the total amount of blood that is in the heart. Normal EF is 50–70%, reduced is 40–50%, and low is <40%. The lower the percent, the more severe the heart failure. The American Heart Association explains more about Ejection Fraction in their short video. Click here to watch the video. Vitals Physical Exam The EKG shows the electrical conduction through your heart. Sometimes small changes in the EKG can be a sign that a heart is getting sicker. Once in a while, your doctor will ask you to wear a Holter monitor, which is like a portable EKG that can monitor for arrhythmias happening throughout the day. An exercise test may also be used to look for arrhythmias during exercise. It can also be helpful to check if your heart is strong enough to keep you active. There are several blood tests doctors use to diagnose heart failure. Most patients have labs drawn at scheduled times. You may have labs drawn more often if your team feels that you need closer surveillance. BNP (Brain Natriuretic Peptide) Renal Panel Liver Function Test Chest X-ray Cardiac Catheterization To see how much physical activity you can do and to check for arrhythmias during exercise, your doctor may ask you to walk up and down the hall, or exercise on a treadmill or bike. Testing
Is Genetic Testing Right for You?
Scroll down to explore more specific types of exams and tests your care team may order.
Echocardiogram & Ejection Fraction
Office Visits
EKG &
Holter MonitorLabs
Cardiac Imaging
Exercise
Stress TestEchocardiogram & Ejection Fraction
Office Visits
Your vital signs are VITAL. Your heart rate and heart rhythm can tell you a lot about how your heart is working. A persistently fast heart rate can be a sign that the heart is getting sicker. In heart failure, your blood pressure needs to be just right. High blood pressure can be hard on a failing heart and low blood pressure can make you light-headed and not feel well.
Your doctor will perform physical exams to check for signs of worsening heart failure. Your doctor can listen to your heart for extra sounds or leaky valves. They will listen to your lungs and feel your liver in your belly as well as your feet and legs to see if you are holding onto too much fluid.EKG & Holter Monitor
Labs

BNP is a hormone that is released from your heart and blood vessels when they are working harder for long periods of time. When there is more BNP in the bloodstream, this can indicate that the heart is overworked or stretched.
A renal panel checks how well the kidneys are working. If they have reduced blood flow because of heart failure, the levels may be elevated.
A liver function test checks how well the liver is working. If the liver is congested or has too much blood backing up from the heart, the levels may be elevated.Cardiac Imaging
Chest X-rays can show your doctor if you have any fluid in your lungs that can be caused by heart failure. X-rays can also show changes to the size and shape of your heart.
Your doctor may ask that you undergo a catheterization (or “cath”). A “cath” is a procedure performed while you are sleepy/sedated. A doctor will use a long IV to measure the pressures inside your heart and lungs that you can’t measure with just a blood pressure cuff. A cath will give you a better understanding of how well your blood is moving around your body. The information taken from a “cath” can be very useful in helping your doctor figure out how best to treat your heart failure.Exercise Stress Test
Echocardiogram & Ejection Fraction
Office Visits
Your vital signs are VITAL. Your heart rate and heart rhythm can tell you a lot about how your heart is working. A persistently fast heart rate can be a sign that the heart is getting sicker. In heart failure, your blood pressure needs to be just right. High blood pressure can be hard on a failing heart and low blood pressure can make you light-headed and not feel well.
Your doctor will perform physical exams to check for signs of worsening heart failure. Your doctor can listen to your heart for extra sounds or leaky valves. They will listen to your lungs and feel your liver in your belly as well as your feet and legs to see if you are holding onto too much fluid.EKG & Holter Monitor
Labs

BNP is a hormone that is released from your heart and blood vessels when they are working harder for long periods of time. When there is more BNP in the bloodstream, this can indicate that the heart is overworked or stretched.
A renal panel checks how well the kidneys are working. If they have reduced blood flow because of heart failure, the levels may be elevated.
A liver function test checks how well the liver is working. If the liver is congested or has too much blood backing up from the heart, the levels may be elevated.Cardiac Imaging
Chest X-rays can show your doctor if you have any fluid in your lungs that can be caused by heart failure. X-rays can also show changes to the size and shape of your heart.
Your doctor may ask that you undergo a catheterization (or “cath”). A “cath” is a procedure performed while you are sleepy/sedated. A doctor will use a long IV to measure the pressures inside your heart and lungs that you can’t measure with just a blood pressure cuff. A cath will give you a better understanding of how well your blood is moving around your body. The information taken from a “cath” can be very useful in helping your doctor figure out how best to treat your heart failure.Exercise Stress Test