-
Overview
-
Types
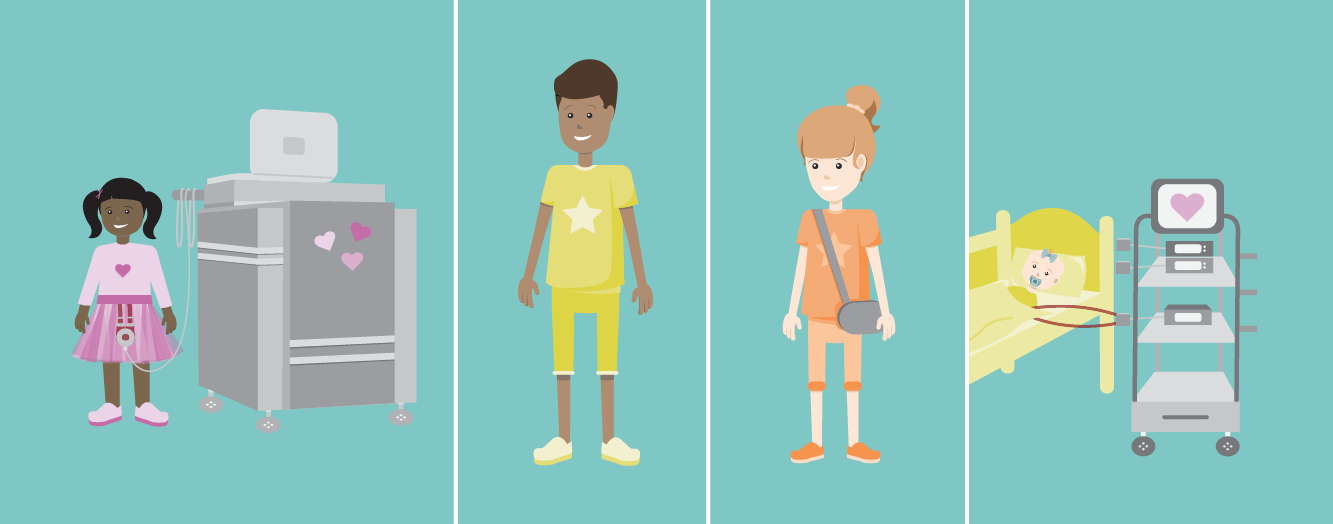
VAD stands for “Ventricular Assist Device.” A VAD is a pump surgically placed in a sick or weak heart to help deliver blood to the body. Children may need a VAD because they are born with a heart problem or because one develops over time. Children with heart failure often have symptoms like feeling short of breath, having trouble eating or gaining weight, and having low energy. A VAD may help these symptoms get better. Sometimes a VAD, depending on the type, will help you feel well enough to leave the hospital and return to school or work. Let’s take a look at your care journey with a VAD. There are many people that will care for you during your VAD journey, but your care team will guide you throughout the entire journey and always help you make decisions about your care. Just remember, you and your caregivers are a very important part of the team. Your care team may include: VADs can be implanted in any chamber of the heart, but usually they’re located in the left ventricle. The location of the device determines what your VAD may be called. A VAD may be used to help a heart pump for many reasons. Depending on your situation, a VAD may be used as a: Although rare, complications may occur while living with a VAD, which may include: Reducing VAD Risks Hearts & Minds: Neurodevelopment in Patients with Heart Failure & VADs A VAD may be used to help a heart pump for many reasons. Depending on your situation, a VAD may be used as a: Although rare, complications may occur while living with a VAD, which may include: Reducing VAD RisksWhat Are VADs?
The Care Journey
Meet the Care Team


Where is the VAD Implanted?
Benefits
Risks
Benefits

Risks

Although the complications above sound scary, there are many steps you and your care team will take to reduce the possibility of complications. VAD patients will:Resources
See Health & Wellness > Life Style > Resources

Although the complications above sound scary, there are many steps you and your care team will take to reduce the possibility of complications. VAD patients will:
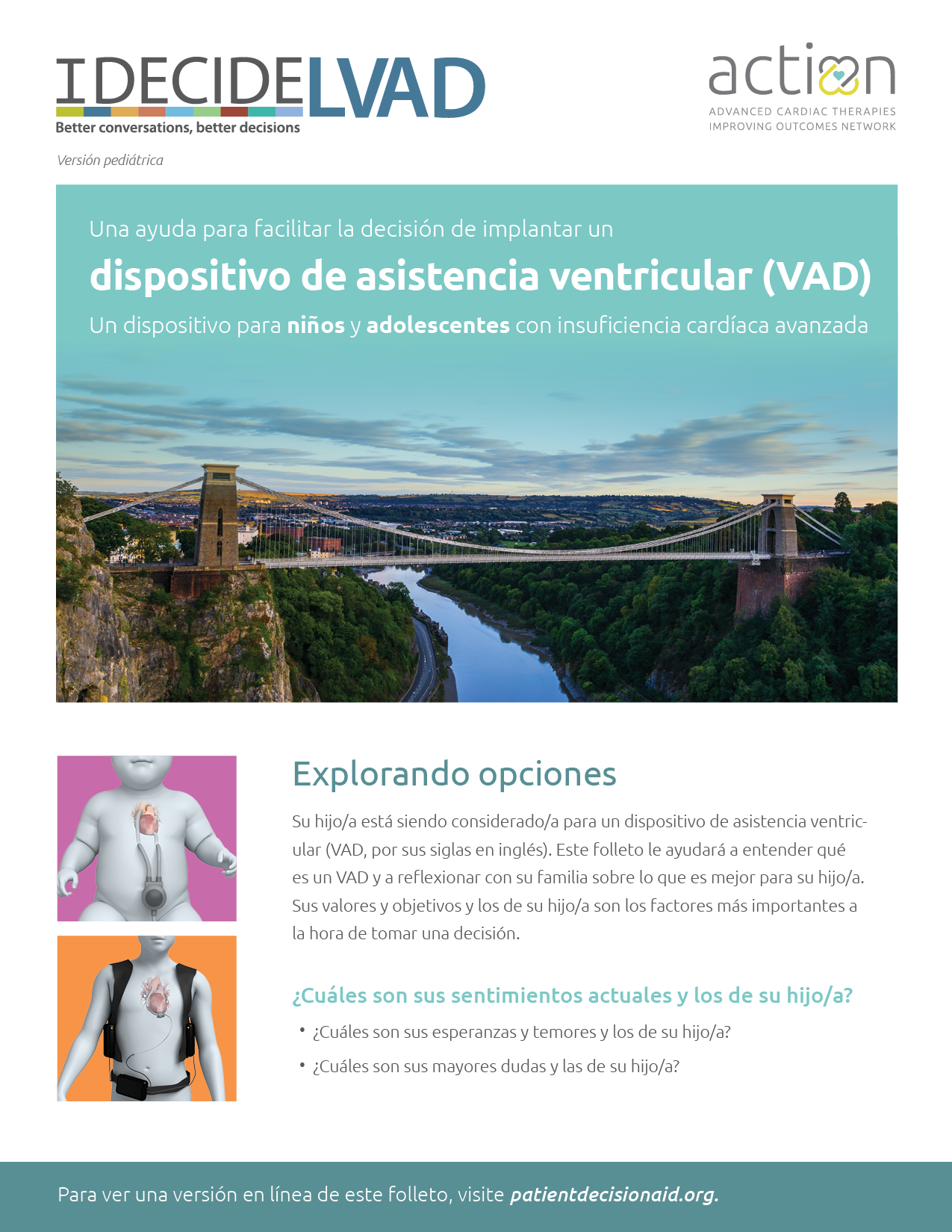
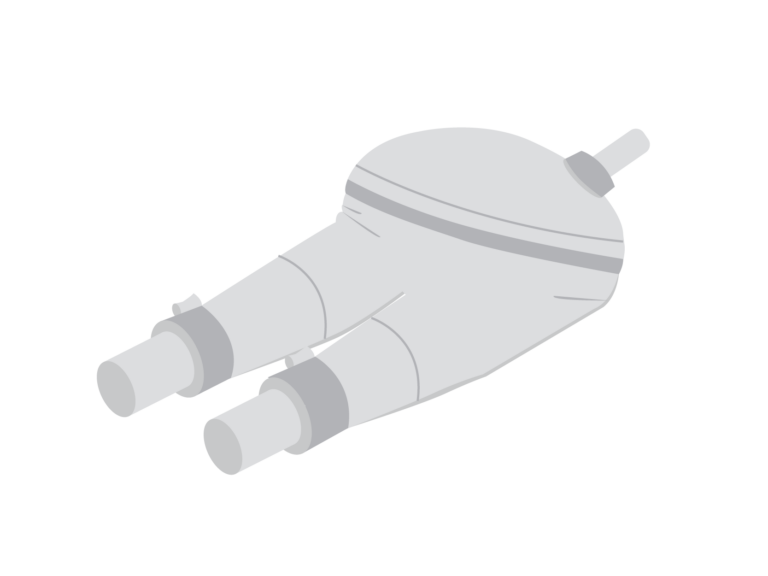
VADs can be defined by the action that they perform. VADs can pump blood by a spinning action (continuous flow VAD) or by a pumping action (pulsatile flow VAD). Check out this pediatric version of the IDecide VAD decision aid booklet. This booklet was designed for pediatric patients and their families to help them better understand VADs and determine which one might be best for their unique situation. Available in both English and Spanish. Pulsatile flow VADs work by pumping blood in and out of a chamber. Air moves a membrane to fill and eject blood from the chambers to the body. The pump is connected to a large machine called a driver. If you have a pulsatile flow VAD, you will have a pulse. Below are common examples of pulsatile flow VADs. Learn about the Berlin Heart EXCOR®,
how it works, the benefits and risks,
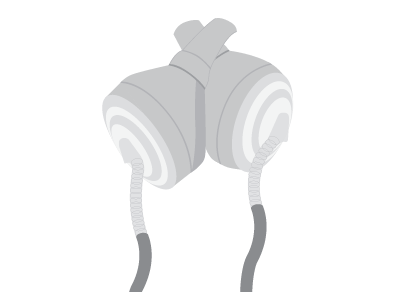
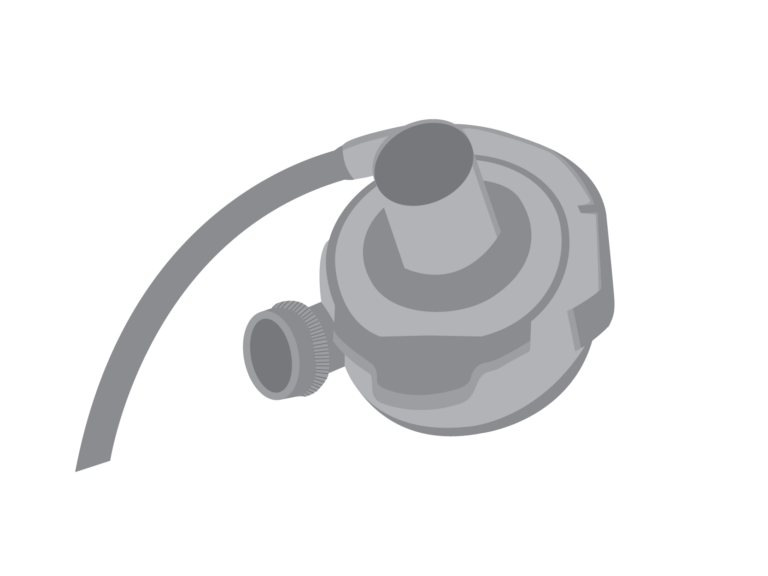
and all about the surgery journey. Learn about the SynCardia Total Artificial Heart (TAH-t), how it works, the benefits and risks, and all about the surgery journey. Continuous flow (CF) VADs work by continuously spinning blood from the weak part of the heart, through the device, out to the aorta, and the rest of the body. There is a small motor located inside the VAD that helps with this spinning motion. The pump is always connected to a controller and requires a power source to keep the VAD spinning. Because the continuous flow device bypasses the weakened heart chamber, you may not be able to feel your pulse. Below are common examples of continuous flow VADs. Learn more about the HeartMate 3™ Learn about the PediMag™ and CentriMag™ Types of VADs
VAD Decision Aid Booklet
Pulsatile
Berlin Heart EXCOR®
SynCardia (TAH-t)
Continuous Flow
HeartMate 3™ LVAD
LVAD, how it works, the benefits and risks,
and all about the surgery journey.PediMag™
& CentriMag™
VADs, how they work, the benefits and risks,
and all about the surgery journey.