PediMag™ & CentriMag™
Overview
Your Surgery Journey
Overview
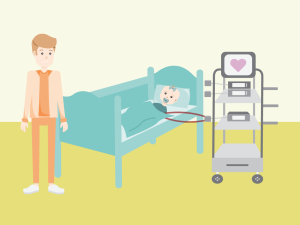
The CentriMag™ and PediMag™ work by continuously spinning blood from the weak part of the heart out to the rest of the body. They are paracorporeal devices, which means soft tubes, called cannulae, are placed inside the heart but connect to a device outside of the body. The CentriMag™ and PediMag™ devices provide proper blood flow so the vital organs get the oxygen and nutrients they need to work properly.
-
Device Components
-
Benefits
-
Risks
Device Components
There are several parts within the CentriMag™ and PediMag™ systems.
Cannula
During VAD surgery, your heart surgeon will place cannulas that are special tubes made of a very soft silicone material. These soft cannulas will come out of your lower chest area just below your breastbone. Your heart has two pumping chambers, a left ventricle and a right ventricle. Your cardiologist and surgeon will decide if you need support on just one ventricle or both. If you only need support for one ventricle, you will have two cannulas. If you need support for both ventricles, you will need four cannulas.
Circuit
The circuit is clear tubing that connects the cannulae to the blood pump allowing the blood to circulate.
Blood Pump
The blood pump is a round disc with fins called an impeller. As the impeller spins, it pulls blood out of the weak ventricle through the circuit and then pushes the blood back out to the rest of the body. There are two different pump sizes. The PediMag™ is the smaller device, generally used for infants and toddlers.
Console
The electronic console allows the care team to control the speed of the impeller, monitor how the device is working and troubleshoot any alarms.
Benefits
 CentriMag™ and PediMag™ can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
CentriMag™ and PediMag™ can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
- Bridge to Transplant: To support the heart until the best donor heart is available for transplant.
- Bridge to Recovery: To support the heart if there is a chance the heart will recover.
- Bridge to Decision: To support the heart until a decision can be made by the family and medical team regarding next steps (surgeries or medications).
A CentriMag™ or PediMag™ may help reduce heart failure symptoms and improve quality of life as you continue along your journey.
Risks
 There are also some risks associated with having a VAD, but your care team will work hard to keep you safe.
There are also some risks associated with having a VAD, but your care team will work hard to keep you safe.
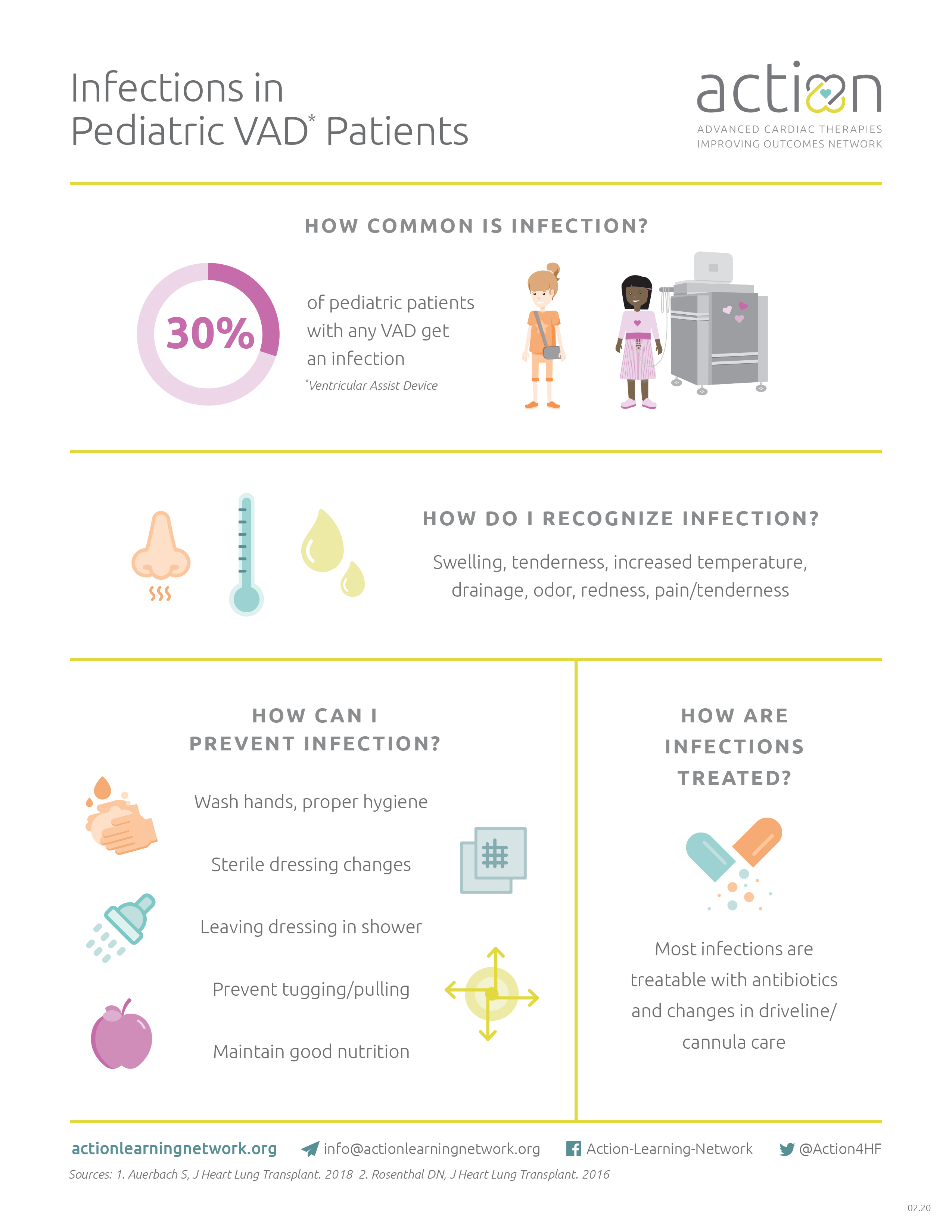
Infection
The soft cannulae come out of your belly and will need to be cleaned frequently. This is important because bacteria lives on your skin and may cause an infection at your cannula site. You may feel nervous the first few times your dressings are changed, but your care team will be there to support you.
Bleeding
There is a risk of bleeding with all VADs, but it is more common with a CentriMag™ or PediMag™. To prevent clots from forming in the device, you have to be on a blood thinner. Sometimes the blood thinner will lead to bleeding that may require a change in medicines, a blood transfusion, or in some cases, a surgery to stop the bleeding. Your care team will manage your blood thinner medicine and levels carefully to try to prevent bleeding. Sometimes, even with perfect levels bleeding will occur.
Stroke
There is a risk of stroke with all VADs. A clot can form in the VAD, become dislodged, and may travel up a blood vessel to the brain. A blood clot in the brain leads to a decreased blood flow to the brain in that specific area, and this is called a stroke. Your care team will manage your blood thinner medicines and levels carefully to try to prevent a stroke. Sometimes, even with perfect levels, a stroke will occur.
Your care team will monitor you for the following symptoms:
- Headache
- Confusion
- Numbness and/or tingling on one side of the body
- Weakness on one side of the body
- Slurred speech
Pediatric VAD Infections
Download the pdf to learn more.
Take ACTION Reducing Stroke Rates
Download the pdf to learn more.
Device Components
There are several parts within the CentriMag™ and PediMag™ systems.
Cannula
During VAD surgery, your heart surgeon will place cannulas that are special tubes made of a very soft silicone material. These soft cannulas will come out of your lower chest area just below your breastbone. Your heart has two pumping chambers, a left ventricle and a right ventricle. Your cardiologist and surgeon will decide if you need support on just one ventricle or both. If you only need support for one ventricle, you will have two cannulas. If you need support for both ventricles, you will need four cannulas.
Circuit
The circuit is clear tubing that connects the cannulae to the blood pump allowing the blood to circulate.
Blood Pump
The blood pump is a round disc with fins called an impeller. As the impeller spins, it pulls blood out of the weak ventricle through the circuit and then pushes the blood back out to the rest of the body. There are two different pump sizes. The PediMag™ is the smaller device, generally used for infants and toddlers.
Console
The electronic console allows the care team to control the speed of the impeller, monitor how the device is working and troubleshoot any alarms.
Benefits
 CentriMag™ and PediMag™ can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
CentriMag™ and PediMag™ can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
- Bridge to Transplant: To support the heart until the best donor heart is available for transplant.
- Bridge to Recovery: To support the heart if there is a chance the heart will recover.
- Bridge to Decision: To support the heart until a decision can be made by the family and medical team regarding next steps (surgeries or medications).
A CentriMag™ or PediMag™ may help reduce heart failure symptoms and improve quality of life as you continue along your journey.
Risks
 There are also some risks associated with having a VAD, but your care team will work hard to keep you safe.
There are also some risks associated with having a VAD, but your care team will work hard to keep you safe.
Infection
The soft cannulae come out of your belly and will need to be cleaned frequently. This is important because bacteria lives on your skin and may cause an infection at your cannula site. You may feel nervous the first few times your dressings are changed, but your care team will be there to support you.
Bleeding
There is a risk of bleeding with all VADs, but it is more common with a CentriMag™ or PediMag™. To prevent clots from forming in the device, you have to be on a blood thinner. Sometimes the blood thinner will lead to bleeding that may require a change in medicines, a blood transfusion, or in some cases, a surgery to stop the bleeding. Your care team will manage your blood thinner medicine and levels carefully to try to prevent bleeding. Sometimes, even with perfect levels bleeding will occur.
Stroke
There is a risk of stroke with all VADs. A clot can form in the VAD, become dislodged, and may travel up a blood vessel to the brain. A blood clot in the brain leads to a decreased blood flow to the brain in that specific area, and this is called a stroke. Your care team will manage your blood thinner medicines and levels carefully to try to prevent a stroke. Sometimes, even with perfect levels, a stroke will occur.
Your care team will monitor you for the following symptoms:
- Headache
- Confusion
- Numbness and/or tingling on one side of the body
- Weakness on one side of the body
- Slurred speech
Pediatric VAD Infections
Download the pdf to learn more.
Take ACTION Reducing Stroke Rates
Download the pdf to learn more.
Your Surgery Journey

Navigating such a big and important surgery can feel overwhelming. There are many people and resources available to help you get through your surgery journey and ultimately get you living a more comfortable and healthy life. You can also prepare by reading and learning as much as you can before heading into surgery.
-
Preparing
for Surgery -
After Surgery
-
Recovery
Preparing for Surgery
 Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.
Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.
Before your surgery, doctors called anesthesiologists will visit you. They are responsible for keeping you asleep during surgery. You will not feel any pain while you are asleep. All you will remember is traveling down to the operating room.
Your Surgery Day
The surgeon performs a sternotomy which involved opening your chest and implanting the cannulae into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation.
After the VAD is turned on, the settings are adjusted to provide the correct blood flow to your body.
After Surgery
 When you wake up from surgery, you will be in the Intensive Care Unit (ICU).
When you wake up from surgery, you will be in the Intensive Care Unit (ICU).
Surgery will make you feel weak and sleepy. For these reasons, you will have a plastic tube in your mouth that will help you breathe. You will also have many special IVs, cables, and drains, which are needed to monitor your VAD and heart function.
This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal.
As with any surgery, you will probably feel some pain afterwards. Once your care team thinks you’re strong enough to be more awake and breathe on your own, your medicines keeping you sleepy will be turned off. Your breathing tube will be removed, and you will be given oxygen using a nasal cannula or mask. Your care team may also decide to give you a boost of nutrition, feeding you through a special tube in your nose called a nasogastric tube.
Recovery Self Care
When your breathing tube is out and you’re fully awake, this is when rehabilitation begins. Specially trained physical and occupational therapists will assist you in getting out of bed for the first time after surgery. Your care team will be there to support you every step of the way.
Your cannula sites will need to have dressing changes using sterile technique. Your care team will use sterile gloves and wear masks during dressing changes. How often your dressings are changed will be determined by your care team.
Recovery is a slow and steady process. Everyday you will gain more strength and your care team will help you make decisions for the next steps in your journey.
Preparing for Surgery
 Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.
Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.
Before your surgery, doctors called anesthesiologists will visit you. They are responsible for keeping you asleep during surgery. You will not feel any pain while you are asleep. All you will remember is traveling down to the operating room.
Your Surgery Day
The surgeon performs a sternotomy which involved opening your chest and implanting the cannulae into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation.
After the VAD is turned on, the settings are adjusted to provide the correct blood flow to your body.
After Surgery
 When you wake up from surgery, you will be in the Intensive Care Unit (ICU).
When you wake up from surgery, you will be in the Intensive Care Unit (ICU).
Surgery will make you feel weak and sleepy. For these reasons, you will have a plastic tube in your mouth that will help you breathe. You will also have many special IVs, cables, and drains, which are needed to monitor your VAD and heart function.
This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal.
As with any surgery, you will probably feel some pain afterwards. Once your care team thinks you’re strong enough to be more awake and breathe on your own, your medicines keeping you sleepy will be turned off. Your breathing tube will be removed, and you will be given oxygen using a nasal cannula or mask. Your care team may also decide to give you a boost of nutrition, feeding you through a special tube in your nose called a nasogastric tube.
Recovery Self Care
When your breathing tube is out and you’re fully awake, this is when rehabilitation begins. Specially trained physical and occupational therapists will assist you in getting out of bed for the first time after surgery. Your care team will be there to support you every step of the way.
Your cannula sites will need to have dressing changes using sterile technique. Your care team will use sterile gloves and wear masks during dressing changes. How often your dressings are changed will be determined by your care team.
Recovery is a slow and steady process. Everyday you will gain more strength and your care team will help you make decisions for the next steps in your journey.