Knowing Your Device and
Understanding Surgery
Over the years, advanced technology has been used to develop devices to help patients diagnosed with heart failure. Many of these devices, although designed for adults, have been adapted for use in children. Let’s explore each device and what to expect before, during, and after surgery.
Over the years, advanced technology has been used to develop devices to help patients diagnosed
with heart failure. Many of these devices, although designed for adults, have been adapted for use
in children. Let’s explore each device and what to expect before, during, and after surgery.
-
1
Pacemaker/ICD
-
3
Pre-Transplant
-
4
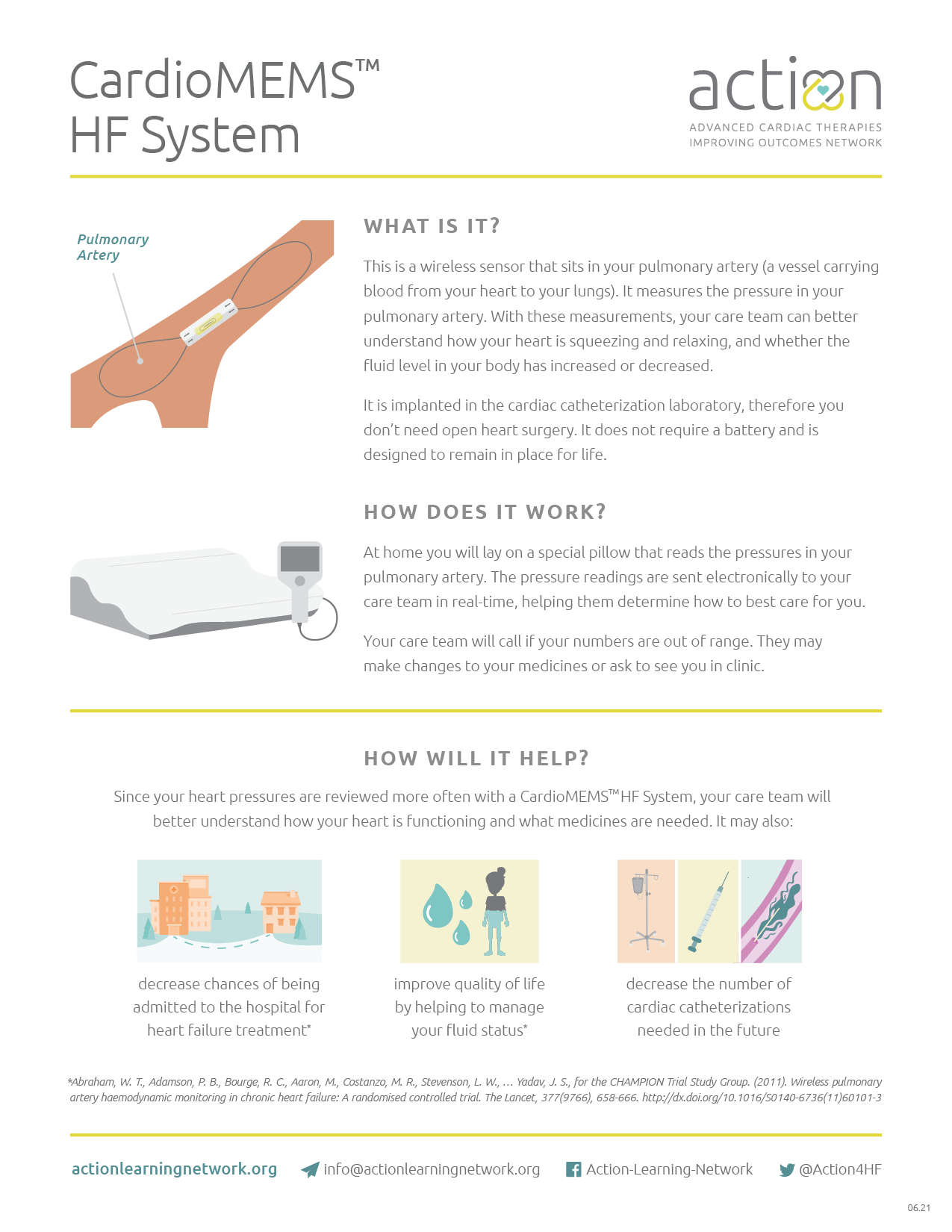
CardioMEMS™
Sometimes patients with heart failure will have abnormal heart rhythms or their doctor feels like they are at increased risk of having a life-threatening heart rhythm. When a heart rhythm isn’t normal (called arrhythmia), it can cause the heart to beat too slowly (bradycardia), too quickly (tachycardia), or abnormally (dysrhythmia). Also, if the pathway is blocked between the upper and lower parts of the heart, the heart may beat at different rates (called a heart block). A pacemaker or automatic implantable cardioverter defibrillator (ICD) can correct the electrical activity and fix abnormal heart rhythms. An arrhythmia can cause symptoms like fluttering in the chest, dizziness, tiredness, or may even cause fainting. Some arrhythmias are life-threatening and may cause the heart to quiver, which prevents blood from getting to the brain and body. This is considered an emergency situation that requires a defibrillator to shock the heart to reset the rhythm immediately. Pacemakers monitor the heart’s rhythm and send a low voltage electrical signal to the heart to “pace” the heart into a correct rhythm. Pacemakers can be used for a short or long amount of time and can be placed internally (inside the body) or externally (outside the body). The short-term external pacemakers are typically used: The long-term internal pacemaker is a small device with wires that lead to the heart chambers. It is implanted into the chest or belly to help the heart beat at a normal rhythm. Pacemakers typically last for many years. Pacemakers deliver low voltage impulses to correct the heart rhythm. However, an ICD detects lethal arrhythmias and delivers high voltage shocks to reset the heart rhythm during a life-threatening emergency. The pacemaker or ICD implant surgery is a minor surgery when placed through a vessel. Often this procedure is done quickly, however times will vary per patient. During the procedure, the surgeon makes an incision into the skin, places the wires inside the heart chambers, and inserts the small device underneath the skin. The pacemaker or ICD is turned on and the settings are adjusted. Afterwards, the incision is closed. There are some restrictions in activity level for a short time after surgery, but normal activity may resume within a few weeks after implant. Benefits of having a Pacemaker/ICD include: Risks related to Pacemaker/ICD surgery include: Benefits of having a Pacemaker/ICD include: Risks related to Pacemaker/ICD surgery include:Overview
 What happens when you turn on a light switch? Electricity travels quickly through wiring that makes a lightbulb glow! The heart works in a similar way. There is a small amount of electricity that moves through a pathway that starts at the top of the heart and travels to the bottom, causing the heart to beat. These electrical signals are called heart rhythms and can be seen when you are connected to an EKG or heart monitor.
What happens when you turn on a light switch? Electricity travels quickly through wiring that makes a lightbulb glow! The heart works in a similar way. There is a small amount of electricity that moves through a pathway that starts at the top of the heart and travels to the bottom, causing the heart to beat. These electrical signals are called heart rhythms and can be seen when you are connected to an EKG or heart monitor.Pacemakers vs ICD

Implanting Your Device
Benefits
Risks
Benefits

Risks



Your HeartMate 3™ LVAD will work by continuously spinning blood from the weak part of the heart, through the device, out to the aorta, and the rest of the body. There is a small rotor located inside the VAD that helps with this spinning motion. The pump is always connected to a controller and requires a power source to keep the VAD spinning. Because the continuous flow device bypasses the weakened heart chamber, you may not be able to feel your pulse. Already have a HeartMate 3™ LVAD? Want more information? Check out the HeartMate 3™ LVAD ACTION Patent Education Handbook. ¿Hablas Español? Aquí está la versión en Español. Are you an ADULT with a HeartMate 3™ LVAD? We created a patient handbook resource for information tailored to adults as well. See the HeartMate 3™ LVAD Adult ACTION Patent Education Handbook. The goal of the VAD is to improve the way you feel. Learn more about how a VAD could improve your quality of life in the interactive below. While VADs have been shown to help many patients, living with a VAD has its challenges. VAD patients must: Learning about your VAD is an important part of getting you discharged and keeping you safe. Watch this video to learn more about how your device works. Your care team will provide you with more in-depth training to prepare for the VAD quiz that you and your caregivers must complete before leaving the hospital. Check out our VAD-Venture Controller Change-Out simulation app for iOS. This simulation game is designed to help you practice changing out the HeartMate 3™ LVAD controller, in return helping you build the confidence needed to properly care for your device. Don’t have iOS? Practice your skills here. The equipment is life-saving and managing it may feel overwhelming. However, learning how each of the pieces work together will help you feel more comfortable in your daily journey. The driveline is made of electrical wires that connect the HeartMate 3™ LVAD to the system controller. The driveline has two important functions in order to make the device work properly. First, the driveline brings power to the HeartMate 3™ LVAD to make the pump spin. If the driveline is ever disconnected from the system controller your HeartMate 3™ LVAD will stop working. Secondly, the driveline sends important information back and forth between the LVAD (inside the heart) and the system controller. You will only be plugged into the monitor when you are in the hospital or in clinic. The monitor tells your care team how your device is working so they can make any adjustments needed. There is a port where the driveline enters the controller and transfers power and information. The controller provides power to the pump, and the pump sends vital information back about how the pump is working. To learn more about your HeartMate 3™ LVAD equipment watch the Equipment interactive below. Pump Parameters To learn more about alarms and troubleshooting, reference your ACTION HeartMate 3™ LVAD Patient Education Handbook, or the HeartMate 3™ Left Ventricular Assist System Patient Handbook given to you on or before your surgery or watch the Learning Alarms & Troubleshooting interactive below. You must avoid being away from electricity for a long period of time. Find out if a continuous flow VAD is right for you. There are also some risks associated with having a VAD, but your care team will work hard to keep you safe. The driveline comes out of your belly and will need to be cleaned frequently. This is important because bacteria lives on your skin and may cause an infection at your driveline site. You may feel nervous the first few times your dressings are changed, but your care team will be there to support you. There is a risk of stroke with all VADs. A clot can form in the VAD, become dislodged, and may travel up a blood vessel to the brain. A blood clot in the brain leads to a decreased blood flow to the brain in that specific area, and this is called a stroke. Your care team will manage your blood thinner medicines and levels carefully to try to prevent a stroke. Sometimes, even with perfect levels, a stroke will occur. Your care team will monitor you for the following symptoms: There is a risk of bleeding with all VADs. To prevent clots from forming in the device, you have to be on a blood thinner. Sometimes the blood thinner will lead to bleeding that may require a change in medicines, a blood transfusion, or in some cases, a surgery to stop the bleeding. Your care team will manage your blood thinner medicine and levels carefully to try to prevent bleeding. Sometimes, even with perfect levels bleeding will occur. Download the pdf to learn more. Download the pdf to learn more. The equipment is life-saving and managing it may feel overwhelming. However, learning how each of the pieces work together will help you feel more comfortable in your daily journey. The driveline is made of electrical wires that connect the HeartMate 3™ LVAD to the system controller. The driveline has two important functions in order to make the device work properly. First, the driveline brings power to the HeartMate 3™ LVAD to make the pump spin. If the driveline is ever disconnected from the system controller your HeartMate 3™ LVAD will stop working. Secondly, the driveline sends important information back and forth between the LVAD (inside the heart) and the system controller. You will only be plugged into the monitor when you are in the hospital or in clinic. The monitor tells your care team how your device is working so they can make any adjustments needed. There is a port where the driveline enters the controller and transfers power and information. The controller provides power to the pump, and the pump sends vital information back about how the pump is working. To learn more about your HeartMate 3™ LVAD equipment watch the Equipment interactive below. Pump Parameters To learn more about alarms and troubleshooting, reference your ACTION HeartMate 3™ LVAD Patient Education Handbook, or the HeartMate 3™ Left Ventricular Assist System Patient Handbook given to you on or before your surgery or watch the Learning Alarms & Troubleshooting interactive below. You must avoid being away from electricity for a long period of time. Find out if a continuous flow VAD is right for you. There are also some risks associated with having a VAD, but your care team will work hard to keep you safe. The driveline comes out of your belly and will need to be cleaned frequently. This is important because bacteria lives on your skin and may cause an infection at your driveline site. You may feel nervous the first few times your dressings are changed, but your care team will be there to support you. There is a risk of stroke with all VADs. A clot can form in the VAD, become dislodged, and may travel up a blood vessel to the brain. A blood clot in the brain leads to a decreased blood flow to the brain in that specific area, and this is called a stroke. Your care team will manage your blood thinner medicines and levels carefully to try to prevent a stroke. Sometimes, even with perfect levels, a stroke will occur. Your care team will monitor you for the following symptoms: There is a risk of bleeding with all VADs. To prevent clots from forming in the device, you have to be on a blood thinner. Sometimes the blood thinner will lead to bleeding that may require a change in medicines, a blood transfusion, or in some cases, a surgery to stop the bleeding. Your care team will manage your blood thinner medicine and levels carefully to try to prevent bleeding. Sometimes, even with perfect levels bleeding will occur. Download the pdf to learn more. Download the pdf to learn more. Navigating such a big and important surgery can feel overwhelming. There are many people and resources available to help get you through surgery and, ultimately, get you living a more comfortable and healthy life. You can also prepare yourself by reading and learning as much as you can before heading into surgery. Learn more about the VAD surgery journey in the interactive below. What should you expect before VAD surgery? Watch the video below to understand what to expect on your HeartMate 3™ LVAD surgery day. Throughout your journey, your care team will support you, guide you, and answer any questions or concerns you have. Everyone’s journey will look a little different. Use the HeartMate 3™ LVAD Patient Journey map to get a feel for what lies ahead. This map will also help you understand when you should be reading and learning about different phases of the journey. There are some important things to consider before starting on your VAD journey. Use these resources to learn more about what lies ahead. How is the VAD implanted in the chest? What should you expect after VAD surgery? Watch the video below to understand what to expect after surgery with a HeartMate 3™ LVAD. After the operation, you will recover in the ICU. You will have a breathing tube that’s connected to a ventilator (breathing machine) and you will be connected to many lines, tubes, and medical equipment. This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal. As with any surgery, you will probably feel some pain afterwards. Learn more about what to expect in the interactive below: The Cardiac Step-Down Unit When you have a VAD there is a lot for you and your caregivers to learn. You will have laboratory testing (labs or bloodwork) done at various scheduled times or whenever your care team feels they need to follow you closer. These labs tell your care team how well your body is functioning with the new device. Click on the image to view a list of possible requested labs. Testing will become part of normal life. Testing will be done at scheduled times and whenever your team feels like you may need closer surveillance. Common tests include: In the hospital, medicine will be given through an IV. Your care team will change those medicines to be given by mouth when preparing for discharge. It’s important the medicines are taken at the same time every day. By the time you are ready to go home, medicines will likely be taken twice a day. Use a pill box to keep your medicines organized. Inform your care team if you take any additional medicines NOT prescribed by them. Learn more about medicines through the interactive below. Blood Thinning Medicines Aspirin Warfarin (Coumadin) Causes for High INR (thin blood): Causes for Low INR (thick blood): Learn more about warfarin (Coumadin) in the Exploring Medicine Treatment Options module and learn more about anticoagulation through the interactive below. High Blood Pressure Medicines Antibiotics Stomach Ulcer & Acid Reflux Medicines Diuretics (medicines to remove extra body water) Most of the following complications are rare and your care team will be with there to help keep you safe. Bleeding Nose Bleeds Gastrointestinal (GI) Bleeds Stroke Hemolysis Learn more about what to look out for in the interactive below: Pump Clots Keeping your blood pressure in a healthy range is very important. Your care team will determine a target blood pressure goal and adjust medicines to meet it. Blood pressure can be monitored using a blood pressure cuff and/ or a Doppler. This depends on if you can feel a pulse. If you go to an outside hospital you may need to tell them the best way to take your blood pressure. Learn more in the interactive below about how your care team will help you stay at a healthy blood pressure. Caring for your driveline will help you avoid getting an infection. Germs that collect at the driveline site could travel to the heart if left untreated. Frequent movement of the driveline can cause damage above and underneath the skin and increase the risk of infection. Using anchors to keep the driveline in place is important to keep the driveline site healthy. If you notice any changes in your driveline or if your driveline gets pulled, tell your care team right away so it can be treated quickly. Signs and symptoms of a driveline infection include: Learn more about what to look out for through the infection interactive below Dressing Changes Learn more about how to properly clean and take care of your driveline in the interactive below. Once you have your VAD, you must stay on a stable diet. Eating a consistent healthy diet will help you heal and get stronger. Fluid balance is very important to maintain VAD flow. Dehydration from not drinking enough or increased fluid losses (vomiting, diarrhea, sweating) will lead to low VAD blood flow. For some patients, having a VAD and needing lots of medical care can be hard. Many patients that have VAD surgery notice an improvement in symptoms while they are in the hospital, but it can take months for you to get stronger and recover. As you recover, you or your caregiver may feel sad, worried, or even angry at times. This is normal. Be honest about how you’re feeling and talk with your care team if you have these feelings or any changes in behavior. Taking care of your emotional and mental health is a very important part of your care. Your care team will be able to connect you with the right support services. As a precaution, always carry your VAD emergency information with you. Driving Precautions Long Distance and Air Travel It will vary from hospital to hospital, but once your care team decides it’s safe for you to return home and go to school or work, or perform your normal activities, multiple steps will occur to ensure your safety. When you do leave the hospital, make sure to: If your care team feels you must stay in the hospital for a longer period of time, you may be able to get school services in the hospital. In-hospital school staff can work with your school to make sure you get the right learning materials. Learn more about how your doctors will determine when you’re ready for jobs and school in the interactive below. If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily. Additional Safety Tips: Check out our VAD-Venture Controller Change-Out simulation app for iOS. This simulation game is designed to help you practice changing out the HeartMate 3™ LVAD controller, in return helping you build the confidence needed to properly care for your device. Don’t have iOS? Practice your skills here. If you are discharged to go home, you will have a detailed communication plan. The plan will include a phone number to call. Your care team will want to hear about most everything. Examples include: Learn more about how to get ready to leave the hospital in the interactive below: Check out our VAD-Venture Controller Change-Out simulation app for iOS. This simulation game is designed to help you practice changing out the HeartMate 3™ LVAD controller, in return helping you build the confidence needed to properly care for your device. Don’t have iOS? Practice your skills here. Medical Safety Card What should you expect before VAD surgery? Watch the video below to understand what to expect on your HeartMate 3™ LVAD surgery day. Throughout your journey, your care team will support you, guide you, and answer any questions or concerns you have. Everyone’s journey will look a little different. Use the HeartMate 3™ LVAD Patient Journey map to get a feel for what lies ahead. This map will also help you understand when you should be reading and learning about different phases of the journey. There are some important things to consider before starting on your VAD journey. Use these resources to learn more about what lies ahead. How is the VAD implanted in the chest? What should you expect after VAD surgery? Watch the video below to understand what to expect after surgery with a HeartMate 3™ LVAD. After the operation, you will recover in the ICU. You will have a breathing tube that’s connected to a ventilator (breathing machine) and you will be connected to many lines, tubes, and medical equipment. This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal. As with any surgery, you will probably feel some pain afterwards. Learn more about what to expect in the interactive below: The Cardiac Step-Down Unit When you have a VAD there is a lot for you and your caregivers to learn. You will have laboratory testing (labs or bloodwork) done at various scheduled times or whenever your care team feels they need to follow you closer. These labs tell your care team how well your body is functioning with the new device. Click on the image to view a list of possible requested labs. Testing will become part of normal life. Testing will be done at scheduled times and whenever your team feels like you may need closer surveillance. Common tests include: In the hospital, medicine will be given through an IV. Your care team will change those medicines to be given by mouth when preparing for discharge. It’s important the medicines are taken at the same time every day. By the time you are ready to go home, medicines will likely be taken twice a day. Use a pill box to keep your medicines organized. Inform your care team if you take any additional medicines NOT prescribed by them. Learn more about medicines through the interactive below. Blood Thinning Medicines Aspirin Warfarin (Coumadin) Causes for High INR (thin blood): Causes for Low INR (thick blood): Learn more about warfarin (Coumadin) in the Exploring Medicine Treatment Options module and learn more about anticoagulation through the interactive below. High Blood Pressure Medicines Antibiotics Stomach Ulcer & Acid Reflux Medicines Diuretics (medicines to remove extra body water) Most of the following complications are rare and your care team will be with there to help keep you safe. Bleeding Nose Bleeds Gastrointestinal (GI) Bleeds Stroke Hemolysis Learn more about what to look out for in the interactive below: Pump Clots Keeping your blood pressure in a healthy range is very important. Your care team will determine a target blood pressure goal and adjust medicines to meet it. Blood pressure can be monitored using a blood pressure cuff and/ or a Doppler. This depends on if you can feel a pulse. If you go to an outside hospital you may need to tell them the best way to take your blood pressure. Learn more in the interactive below about how your care team will help you stay at a healthy blood pressure. Caring for your driveline will help you avoid getting an infection. Germs that collect at the driveline site could travel to the heart if left untreated. Frequent movement of the driveline can cause damage above and underneath the skin and increase the risk of infection. Using anchors to keep the driveline in place is important to keep the driveline site healthy. If you notice any changes in your driveline or if your driveline gets pulled, tell your care team right away so it can be treated quickly. Signs and symptoms of a driveline infection include: Learn more about what to look out for through the infection interactive below Dressing Changes Learn more about how to properly clean and take care of your driveline in the interactive below. Once you have your VAD, you must stay on a stable diet. Eating a consistent healthy diet will help you heal and get stronger. Fluid balance is very important to maintain VAD flow. Dehydration from not drinking enough or increased fluid losses (vomiting, diarrhea, sweating) will lead to low VAD blood flow. For some patients, having a VAD and needing lots of medical care can be hard. Many patients that have VAD surgery notice an improvement in symptoms while they are in the hospital, but it can take months for you to get stronger and recover. As you recover, you or your caregiver may feel sad, worried, or even angry at times. This is normal. Be honest about how you’re feeling and talk with your care team if you have these feelings or any changes in behavior. Taking care of your emotional and mental health is a very important part of your care. Your care team will be able to connect you with the right support services. As a precaution, always carry your VAD emergency information with you. Driving Precautions Long Distance and Air Travel It will vary from hospital to hospital, but once your care team decides it’s safe for you to return home and go to school or work, or perform your normal activities, multiple steps will occur to ensure your safety. When you do leave the hospital, make sure to: If your care team feels you must stay in the hospital for a longer period of time, you may be able to get school services in the hospital. In-hospital school staff can work with your school to make sure you get the right learning materials. Learn more about how your doctors will determine when you’re ready for jobs and school in the interactive below. If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily. Additional Safety Tips: Check out our VAD-Venture Controller Change-Out simulation app for iOS. This simulation game is designed to help you practice changing out the HeartMate 3™ LVAD controller, in return helping you build the confidence needed to properly care for your device. Don’t have iOS? Practice your skills here. If you are discharged to go home, you will have a detailed communication plan. The plan will include a phone number to call. Your care team will want to hear about most everything. Examples include: Learn more about how to get ready to leave the hospital in the interactive below: Check out our VAD-Venture Controller Change-Out simulation app for iOS. This simulation game is designed to help you practice changing out the HeartMate 3™ LVAD controller, in return helping you build the confidence needed to properly care for your device. Don’t have iOS? Practice your skills here. Medical Safety Card Medtronic has stopped the distribution and sale of the HVAD™ System as of June 3, 2021(see full press release). Children and young adults who are currently supported with an HVAD™ System will receive the same excellent care from their care teams. Our ACTION education material is still relevant for those supported by the HVAD™ System. Contact your care team with any questions. The HVAD™ System will work by continuously spinning blood from the weak part of the heart, through the device, out to the aorta, and the rest of the body. There is a small impeller located inside the VAD that helps with this spinning motion. The pump is always connected to a controller and a power source that keeps the VAD spinning. Because the continuous flow device bypasses the weakened heart chamber, you may not be able to feel your pulse. Want more information? See our HVAD™ System ACTION Patent Education Handbook. While VADs have been shown to help many patients, living with a VAD has its challenges. VAD patients must: Learning about your VAD is an important part of getting you discharged and keeping you safe. Watch this video to learn more about how your device works: Your care team will provide you with more in-depth training to prepare for the VAD quiz that you and your caregivers must complete before leaving the hospital. The equipment is life-saving and managing it may feel overwhelming. However, learning how each of the pieces work together will help you feel more comfortable in your daily journey. The driveline cord is filled with electrical wires that connect the HVAD to the controller (the brains of the HVAD). This cord performs two functions to help the device work properly. The HVAD (inside the heart) transfers important information to the controller through the driveline. The driveline also brings power back to the pump to make the HVAD spin. Never disconnect your driveline because this would make your pump stop. You will only be plugged into the monitor when you are in the hospital or in a clinic. The monitor tells your care team how your device is working so they can make any adjustments needed. There is a port where the driveline enters the controller and transfers power and information. The controller provides power to the pump, and the pump sends vital information back about how the pump is working. Pump Parameters To learn more about alarms and troubleshooting, reference your ACTION HVAD™ System Patient Education Handbook, or the HeartWare™ HVAD™ System Patient Manual given to you on or before your surgery or watch the Learning Alarms & Troubleshooting interactive below. You must avoid being away from electricity for a long period of time. A HVAD™ System can be used to help a heart pump for many reasons. Depending on your situation, it may be used as: A HVAD™ System may help reduce heart failure symptoms and improve quality of life as you continue along your journey. Find out if a continuous flow HVAD™ System is right for you. There are also some risks associated with having a VAD, but your care team will work hard to keep you safe. The driveline comes out of your belly and will need to be cleaned frequently. This is important because bacteria lives on your skin and may cause an infection at your driveline site. You may feel nervous the first few times your dressings are changed, but your care team will be there to support you. There is a risk of stroke with all VADs. A clot can form in the VAD, become dislodged, and may travel up a blood vessel to the brain. A blood clot in the brain leads to a decreased blood flow to the brain in that specific area, and this is called a stroke. Your care team will manage your blood thinner medicines and levels carefully to try to prevent a stroke. Sometimes, even with perfect levels, a stroke will occur. Your care team will monitor you for the following symptoms: There is a risk of bleeding with all VADs. To prevent clots from forming in the device, you have to be on a blood thinner. Sometimes the blood thinner will lead to bleeding that may require a change in medicines, a blood transfusion, or in some cases, a surgery to stop the bleeding. Your care team will manage your blood thinner medicine and levels carefully to try to prevent bleeding. Sometimes, even with perfect levels bleeding will occur. Download the pdf to learn more. Download the pdf to learn more. The equipment is life-saving and managing it may feel overwhelming. However, learning how each of the pieces work together will help you feel more comfortable in your daily journey. The driveline cord is filled with electrical wires that connect the HVAD to the controller (the brains of the HVAD). This cord performs two functions to help the device work properly. The HVAD (inside the heart) transfers important information to the controller through the driveline. The driveline also brings power back to the pump to make the HVAD spin. Never disconnect your driveline because this would make your pump stop. You will only be plugged into the monitor when you are in the hospital or in a clinic. The monitor tells your care team how your device is working so they can make any adjustments needed. There is a port where the driveline enters the controller and transfers power and information. The controller provides power to the pump, and the pump sends vital information back about how the pump is working. Pump Parameters To learn more about alarms and troubleshooting, reference your ACTION HVAD™ System Patient Education Handbook, or the HeartWare™ HVAD™ System Patient Manual given to you on or before your surgery or watch the Learning Alarms & Troubleshooting interactive below. You must avoid being away from electricity for a long period of time. A HVAD™ System can be used to help a heart pump for many reasons. Depending on your situation, it may be used as: A HVAD™ System may help reduce heart failure symptoms and improve quality of life as you continue along your journey. Find out if a continuous flow HVAD™ System is right for you. There are also some risks associated with having a VAD, but your care team will work hard to keep you safe. The driveline comes out of your belly and will need to be cleaned frequently. This is important because bacteria lives on your skin and may cause an infection at your driveline site. You may feel nervous the first few times your dressings are changed, but your care team will be there to support you. There is a risk of stroke with all VADs. A clot can form in the VAD, become dislodged, and may travel up a blood vessel to the brain. A blood clot in the brain leads to a decreased blood flow to the brain in that specific area, and this is called a stroke. Your care team will manage your blood thinner medicines and levels carefully to try to prevent a stroke. Sometimes, even with perfect levels, a stroke will occur. Your care team will monitor you for the following symptoms: There is a risk of bleeding with all VADs. To prevent clots from forming in the device, you have to be on a blood thinner. Sometimes the blood thinner will lead to bleeding that may require a change in medicines, a blood transfusion, or in some cases, a surgery to stop the bleeding. Your care team will manage your blood thinner medicine and levels carefully to try to prevent bleeding. Sometimes, even with perfect levels bleeding will occur. Download the pdf to learn more. Download the pdf to learn more. Navigating such a big and important surgery can feel overwhelming. There are many people and resources available to help get you through surgery and, ultimately, get you living a more comfortable and healthy life. You can also prepare yourself by reading and learning as much as you can before heading into surgery. Learn more about the HVAD surgery journey: What should you expect before VAD surgery? Watch the video below to understand what to expect on your HVAD™ System surgery day. Throughout your journey, your care team will support you, guide you, and answer any questions or concerns you have. Everyone’s journey will look a little different. Use the HVAD™ System Patient Journey map to get a feel for what lies ahead. This map will also help you understand when you should be reading and learning about different phases of the journey. There are some important things to consider before starting on your journey. Use these resources to learn more about what lies ahead. How is the HVAD implanted in the chest? Explore this interactive to learn more about the surgery. What should you expect after VAD surgery? Watch the video below to understand what to expect after surgery with a HVAD™ System. After the operation, you will recover in the ICU. You will have a breathing tube that’s connected to a ventilator (breathing machine) and you will be connected to many lines, tubes, and medical equipment. This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal. As with any surgery, you will probably feel some pain afterwards. Learn more about what to expect in the interactive below: The Cardiac Step-Down Unit When you have a VAD there is a lot for you and your caregivers to learn. You will have laboratory testing (labs or bloodwork) done at various scheduled times or whenever your care team feels they need to follow you closer. These labs tell your care team how well your body is functioning with the new device. Click on the image to view a list of possible requested labs. Testing will become part of normal life. Testing will be done at scheduled times and whenever your team feels like you may need closer surveillance. Common tests include: Aspirin Warfarin (Coumadin) Causes for High INR (thin blood): Causes for Low INR (thick blood): Learn more about warfarin (Coumadin) in the Exploring Medicine Treatment Options module and learn more about anticoagulation through the interactive below. High Blood Pressure Medicines Antibiotics Stomach Ulcer & Acid Reflux Medicines Diuretics (medicines to remove extra body water) Most of the following complications are rare and your care team will be with there to help keep you safe. Bleeding Nose Bleeds Gastrointestinal (GI) Bleeds Stroke Hemolysis Learn more about what to look out for in the interactive below: Pump Clots Keeping your blood pressure in a healthy range is very important. Your care team will determine a target blood pressure goal and adjust medicines to meet it. Blood pressure can be monitored using a blood pressure cuff and/ or a Doppler. This depends on if you can feel a pulse. If you go to an outside hospital you may need to tell them the best way to take your blood pressure. Learn more in the interactive below about how your care team will help you stay at a healthy blood pressure. Caring for your driveline will help you avoid getting an infection. Germs that collect at the driveline site could travel to the heart if left untreated. Frequent movement of the driveline can cause damage above and underneath the skin and increase the risk of infection. Using anchors to keep the driveline in place is important to keep the driveline site healthy. If you notice any changes in your driveline or if your driveline gets pulled, tell your care team right away so it can be treated quickly. Signs and symptoms of a driveline infection include: Learn more about what to look out for through the infection interactive below Dressing Changes Learn more about how to properly clean and take care of your driveline in the interactive below. Once you have your VAD, you must stay on a stable diet. Eating a consistent healthy diet will help you heal and get stronger. Fluid balance is very important to maintain VAD flow. Dehydration from not drinking enough or increased fluid losses (vomiting, diarrhea, sweating) will lead to low VAD blood flow. For some patients, having a VAD and needing lots of medical care can be hard. Many patients that have VAD surgery notice an improvement in symptoms while they are in the hospital, but it can take months for you to get stronger and recover. As you recover, you or your caregiver may feel sad, worried, or even angry at times. This is normal. Be honest about how you’re feeling and talk with your care team if you have these feelings or any changes in behavior. Taking care of your emotional and mental health is a very important part of your care. Your care team will be able to connect you with the right support services. There are many things to learn about your new VAD. Watch the video below for tips to keep you safe. You must always have back up equipment with you in case something happens to one of your VAD components. The following items should be with you at all times: As a precaution, always carry your VAD emergency information with you. Driving Precautions Long Distance and Air Travel It will vary from hospital to hospital, but once your care team decides it’s safe for you to return home and go to school or work, or perform your normal activities, multiple steps will occur to ensure your safety. When you do leave the hospital, make sure to: Additional Safety Tips: Learn more about how to get ready to leave the hospital in the interactive below: Emergency Medical Safety Card What should you expect before VAD surgery? Watch the video below to understand what to expect on your HVAD™ System surgery day. Throughout your journey, your care team will support you, guide you, and answer any questions or concerns you have. Everyone’s journey will look a little different. Use the HVAD™ System Patient Journey map to get a feel for what lies ahead. This map will also help you understand when you should be reading and learning about different phases of the journey. There are some important things to consider before starting on your journey. Use these resources to learn more about what lies ahead. How is the HVAD implanted in the chest? Explore this interactive to learn more about the surgery. What should you expect after VAD surgery? Watch the video below to understand what to expect after surgery with a HVAD™ System. After the operation, you will recover in the ICU. You will have a breathing tube that’s connected to a ventilator (breathing machine) and you will be connected to many lines, tubes, and medical equipment. This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal. As with any surgery, you will probably feel some pain afterwards. Learn more about what to expect in the interactive below: The Cardiac Step-Down Unit When you have a VAD there is a lot for you and your caregivers to learn. You will have laboratory testing (labs or bloodwork) done at various scheduled times or whenever your care team feels they need to follow you closer. These labs tell your care team how well your body is functioning with the new device. Click on the image to view a list of possible requested labs. Testing will become part of normal life. Testing will be done at scheduled times and whenever your team feels like you may need closer surveillance. Common tests include: Aspirin Warfarin (Coumadin) Causes for High INR (thin blood): Causes for Low INR (thick blood): Learn more about warfarin (Coumadin) in the Exploring Medicine Treatment Options module and learn more about anticoagulation through the interactive below. High Blood Pressure Medicines Antibiotics Stomach Ulcer & Acid Reflux Medicines Diuretics (medicines to remove extra body water) Most of the following complications are rare and your care team will be with there to help keep you safe. Bleeding Nose Bleeds Gastrointestinal (GI) Bleeds Stroke Hemolysis Learn more about what to look out for in the interactive below: Pump Clots Keeping your blood pressure in a healthy range is very important. Your care team will determine a target blood pressure goal and adjust medicines to meet it. Blood pressure can be monitored using a blood pressure cuff and/ or a Doppler. This depends on if you can feel a pulse. If you go to an outside hospital you may need to tell them the best way to take your blood pressure. Learn more in the interactive below about how your care team will help you stay at a healthy blood pressure. Caring for your driveline will help you avoid getting an infection. Germs that collect at the driveline site could travel to the heart if left untreated. Frequent movement of the driveline can cause damage above and underneath the skin and increase the risk of infection. Using anchors to keep the driveline in place is important to keep the driveline site healthy. If you notice any changes in your driveline or if your driveline gets pulled, tell your care team right away so it can be treated quickly. Signs and symptoms of a driveline infection include: Learn more about what to look out for through the infection interactive below Dressing Changes Learn more about how to properly clean and take care of your driveline in the interactive below. Once you have your VAD, you must stay on a stable diet. Eating a consistent healthy diet will help you heal and get stronger. Fluid balance is very important to maintain VAD flow. Dehydration from not drinking enough or increased fluid losses (vomiting, diarrhea, sweating) will lead to low VAD blood flow. For some patients, having a VAD and needing lots of medical care can be hard. Many patients that have VAD surgery notice an improvement in symptoms while they are in the hospital, but it can take months for you to get stronger and recover. As you recover, you or your caregiver may feel sad, worried, or even angry at times. This is normal. Be honest about how you’re feeling and talk with your care team if you have these feelings or any changes in behavior. Taking care of your emotional and mental health is a very important part of your care. Your care team will be able to connect you with the right support services. There are many things to learn about your new VAD. Watch the video below for tips to keep you safe. You must always have back up equipment with you in case something happens to one of your VAD components. The following items should be with you at all times: As a precaution, always carry your VAD emergency information with you. Driving Precautions Long Distance and Air Travel It will vary from hospital to hospital, but once your care team decides it’s safe for you to return home and go to school or work, or perform your normal activities, multiple steps will occur to ensure your safety. When you do leave the hospital, make sure to: Additional Safety Tips: Learn more about how to get ready to leave the hospital in the interactive below: Emergency Medical Safety Card The CentriMag™ and PediMag™ work by continuously spinning blood from the weak part of the heart out to the rest of the body. They are paracorporeal devices, which means soft tubes, called cannulae, are placed inside the heart but connect to a device outside of the body. The CentriMag™ and PediMag™ devices provide proper blood flow so the vital organs get the oxygen and nutrients they need to work properly. There are several parts within the CentriMag™ and PediMag™ systems. During VAD surgery, your heart surgeon will place cannulas that are special tubes made of a very soft silicone material. These soft cannulas will come out of your lower chest area just below your breastbone. Your heart has two pumping chambers, a left ventricle and a right ventricle. Your cardiologist and surgeon will decide if you need support on just one ventricle or both. If you only need support for one ventricle, you will have two cannulas. If you need support for both ventricles, you will need four cannulas. The circuit is clear tubing that connects the cannulae to the blood pump allowing the blood to circulate. The blood pump is a round disc with fins called an impeller. As the impeller spins, it pulls blood out of the weak ventricle through the circuit and then pushes the blood back out to the rest of the body. There are two different pump sizes. The PediMag™ is the smaller device, generally used for infants and toddlers. The electronic console allows the care team to control the speed of the impeller, monitor how the device is working and troubleshoot any alarms. A CentriMag™ or PediMag™ may help reduce heart failure symptoms and improve quality of life as you continue along your journey. The soft cannulae come out of your belly and will need to be cleaned frequently. This is important because bacteria lives on your skin and may cause an infection at your cannula site. You may feel nervous the first few times your dressings are changed, but your care team will be there to support you. There is a risk of bleeding with all VADs, but it is more common with a CentriMag™ or PediMag™. To prevent clots from forming in the device, you have to be on a blood thinner. Sometimes the blood thinner will lead to bleeding that may require a change in medicines, a blood transfusion, or in some cases, a surgery to stop the bleeding. Your care team will manage your blood thinner medicine and levels carefully to try to prevent bleeding. Sometimes, even with perfect levels bleeding will occur. There is a risk of stroke with all VADs. A clot can form in the VAD, become dislodged, and may travel up a blood vessel to the brain. A blood clot in the brain leads to a decreased blood flow to the brain in that specific area, and this is called a stroke. Your care team will manage your blood thinner medicines and levels carefully to try to prevent a stroke. Sometimes, even with perfect levels, a stroke will occur. Your care team will monitor you for the following symptoms: Download the pdf to learn more. Download the pdf to learn more. There are several parts within the CentriMag™ and PediMag™ systems. During VAD surgery, your heart surgeon will place cannulas that are special tubes made of a very soft silicone material. These soft cannulas will come out of your lower chest area just below your breastbone. Your heart has two pumping chambers, a left ventricle and a right ventricle. Your cardiologist and surgeon will decide if you need support on just one ventricle or both. If you only need support for one ventricle, you will have two cannulas. If you need support for both ventricles, you will need four cannulas. The circuit is clear tubing that connects the cannulae to the blood pump allowing the blood to circulate. The blood pump is a round disc with fins called an impeller. As the impeller spins, it pulls blood out of the weak ventricle through the circuit and then pushes the blood back out to the rest of the body. There are two different pump sizes. The PediMag™ is the smaller device, generally used for infants and toddlers. The electronic console allows the care team to control the speed of the impeller, monitor how the device is working and troubleshoot any alarms. A CentriMag™ or PediMag™ may help reduce heart failure symptoms and improve quality of life as you continue along your journey. The soft cannulae come out of your belly and will need to be cleaned frequently. This is important because bacteria lives on your skin and may cause an infection at your cannula site. You may feel nervous the first few times your dressings are changed, but your care team will be there to support you. There is a risk of bleeding with all VADs, but it is more common with a CentriMag™ or PediMag™. To prevent clots from forming in the device, you have to be on a blood thinner. Sometimes the blood thinner will lead to bleeding that may require a change in medicines, a blood transfusion, or in some cases, a surgery to stop the bleeding. Your care team will manage your blood thinner medicine and levels carefully to try to prevent bleeding. Sometimes, even with perfect levels bleeding will occur. There is a risk of stroke with all VADs. A clot can form in the VAD, become dislodged, and may travel up a blood vessel to the brain. A blood clot in the brain leads to a decreased blood flow to the brain in that specific area, and this is called a stroke. Your care team will manage your blood thinner medicines and levels carefully to try to prevent a stroke. Sometimes, even with perfect levels, a stroke will occur. Your care team will monitor you for the following symptoms: Download the pdf to learn more. Download the pdf to learn more. Navigating such a big and important surgery can feel overwhelming. There are many people and resources available to help you get through your surgery journey and ultimately get you living a more comfortable and healthy life. You can also prepare by reading and learning as much as you can before heading into surgery. Before your surgery, doctors called anesthesiologists will visit you. They are responsible for keeping you asleep during surgery. You will not feel any pain while you are asleep. All you will remember is traveling down to the operating room. The surgeon performs a sternotomy which involved opening your chest and implanting the cannulae into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation. After the VAD is turned on, the settings are adjusted to provide the correct blood flow to your body. Surgery will make you feel weak and sleepy. For these reasons, you will have a plastic tube in your mouth that will help you breathe. You will also have many special IVs, cables, and drains, which are needed to monitor your VAD and heart function. This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal. As with any surgery, you will probably feel some pain afterwards. Once your care team thinks you’re strong enough to be more awake and breathe on your own, your medicines keeping you sleepy will be turned off. Your breathing tube will be removed, and you will be given oxygen using a nasal cannula or mask. Your care team may also decide to give you a boost of nutrition, feeding you through a special tube in your nose called a nasogastric tube. When your breathing tube is out and you’re fully awake, this is when rehabilitation begins. Specially trained physical and occupational therapists will assist you in getting out of bed for the first time after surgery. Your care team will be there to support you every step of the way. Your cannula sites will need to have dressing changes using sterile technique. Your care team will use sterile gloves and wear masks during dressing changes. How often your dressings are changed will be determined by your care team. Recovery is a slow and steady process. Everyday you will gain more strength and your care team will help you make decisions for the next steps in your journey. Before your surgery, doctors called anesthesiologists will visit you. They are responsible for keeping you asleep during surgery. You will not feel any pain while you are asleep. All you will remember is traveling down to the operating room. The surgeon performs a sternotomy which involved opening your chest and implanting the cannulae into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation. After the VAD is turned on, the settings are adjusted to provide the correct blood flow to your body. Surgery will make you feel weak and sleepy. For these reasons, you will have a plastic tube in your mouth that will help you breathe. You will also have many special IVs, cables, and drains, which are needed to monitor your VAD and heart function. This medical equipment is necessary to monitor you and give you the medicines needed for recovery. All the equipment and lines can be startling to see, but they are completely normal. Day by day, your care team will work toward removing lines and tubes. It is also important to get you moving soon after surgery. Getting out of bed as soon as possible will help your body heal. As with any surgery, you will probably feel some pain afterwards. Once your care team thinks you’re strong enough to be more awake and breathe on your own, your medicines keeping you sleepy will be turned off. Your breathing tube will be removed, and you will be given oxygen using a nasal cannula or mask. Your care team may also decide to give you a boost of nutrition, feeding you through a special tube in your nose called a nasogastric tube. When your breathing tube is out and you’re fully awake, this is when rehabilitation begins. Specially trained physical and occupational therapists will assist you in getting out of bed for the first time after surgery. Your care team will be there to support you every step of the way. Your cannula sites will need to have dressing changes using sterile technique. Your care team will use sterile gloves and wear masks during dressing changes. How often your dressings are changed will be determined by your care team. Recovery is a slow and steady process. Everyday you will gain more strength and your care team will help you make decisions for the next steps in your journey.HeartMate 3™ LVAD
Overview
Your Surgery Journey
Overview

 Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!
Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!
Device Components
Benefits
Risks
Device Components
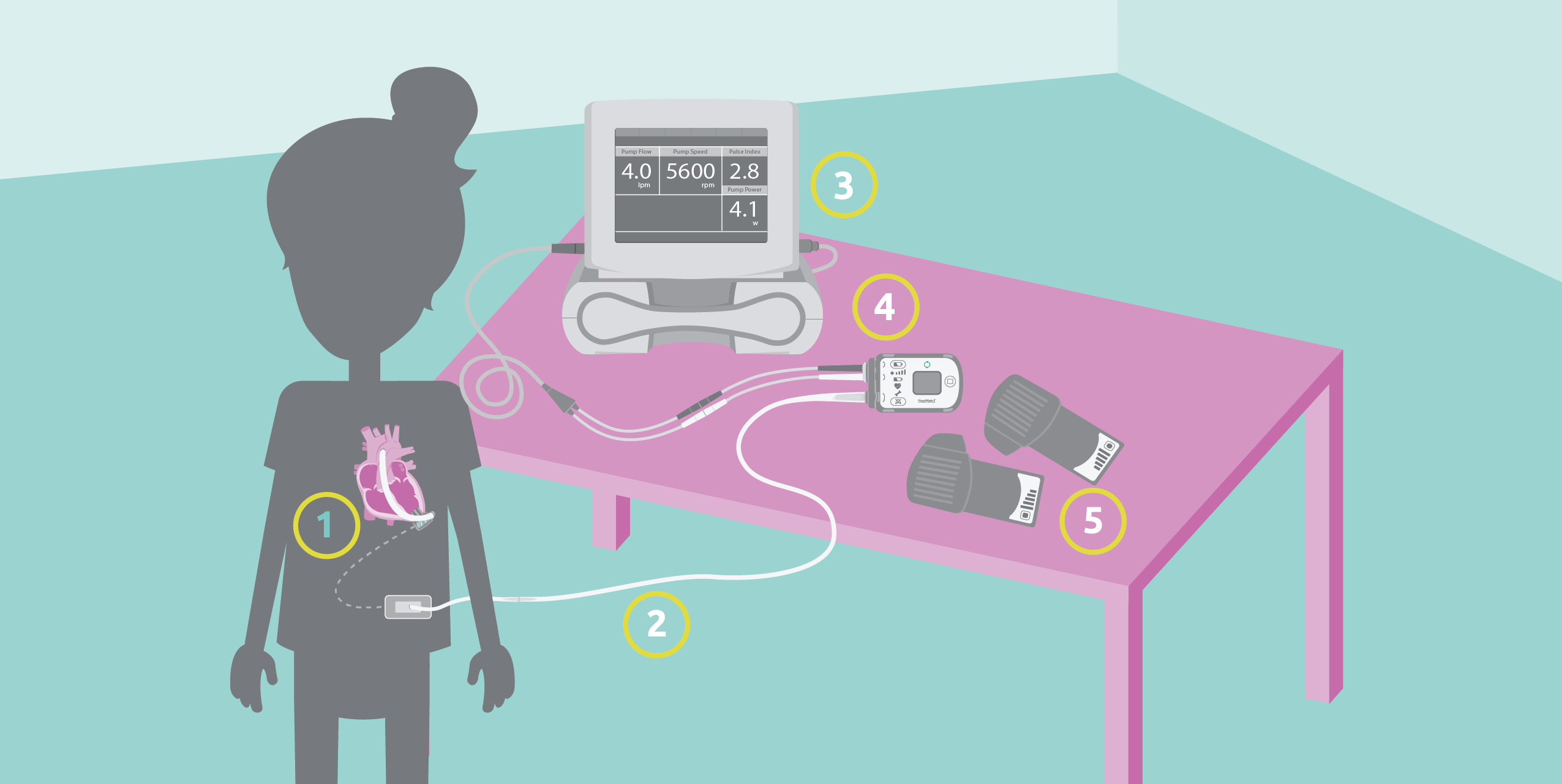
1 VAD
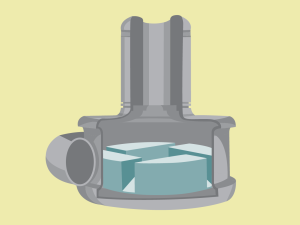
The HeartMate 3™ LVAD is placed inside your chest. The outflow graft is a flexible tube that connects the outflow of the HeartMate 3™ LVAD to the aorta. It helps carry the blood from the pump to the rest of the body. The inside of the pump has a rotor that spins continuously and can distribute up to 10 liters of blood per minute (L/min). 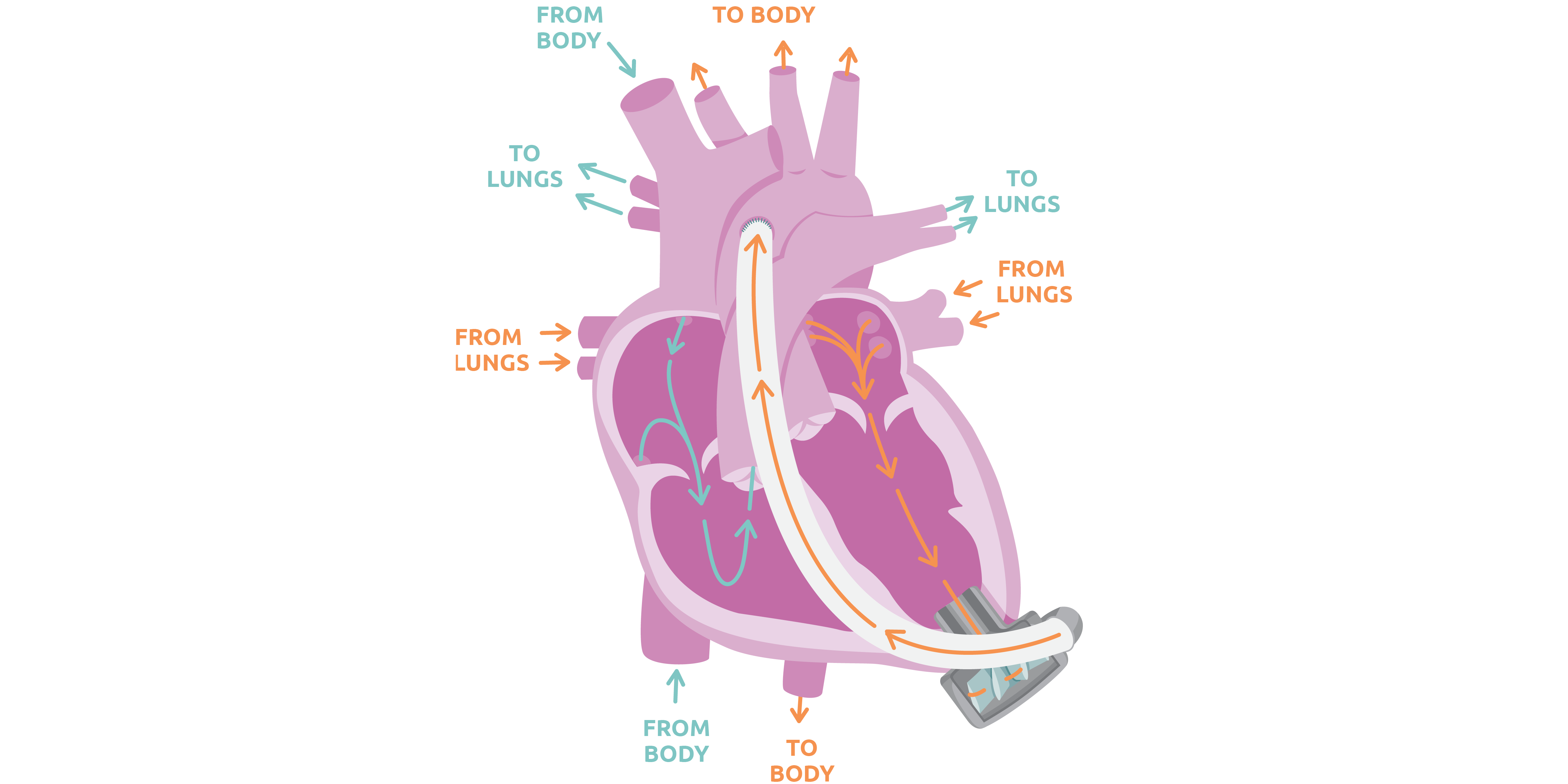
2 Driveline
3 System Monitor
4 System Controller

There are many numbers that you will want to know about. The RPM, or rotations per minute, is set by your care team. The other numbers are calculated but will tell the team a lot about how you are doing. Watch the interactive below to learn more.5 Electrical Power
Benefits
 HeartMate 3™ LVAD can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
HeartMate 3™ LVAD can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
A HeartMate 3™ LVAD may help reduce heart failure symptoms and improve quality of life as you continue along your journey. Is this VAD Right for Me?
Risks

Infection
Stroke
Bleeding
Pediatric VAD Infections
Take ACTION Reducing Stroke Rates
Device Components
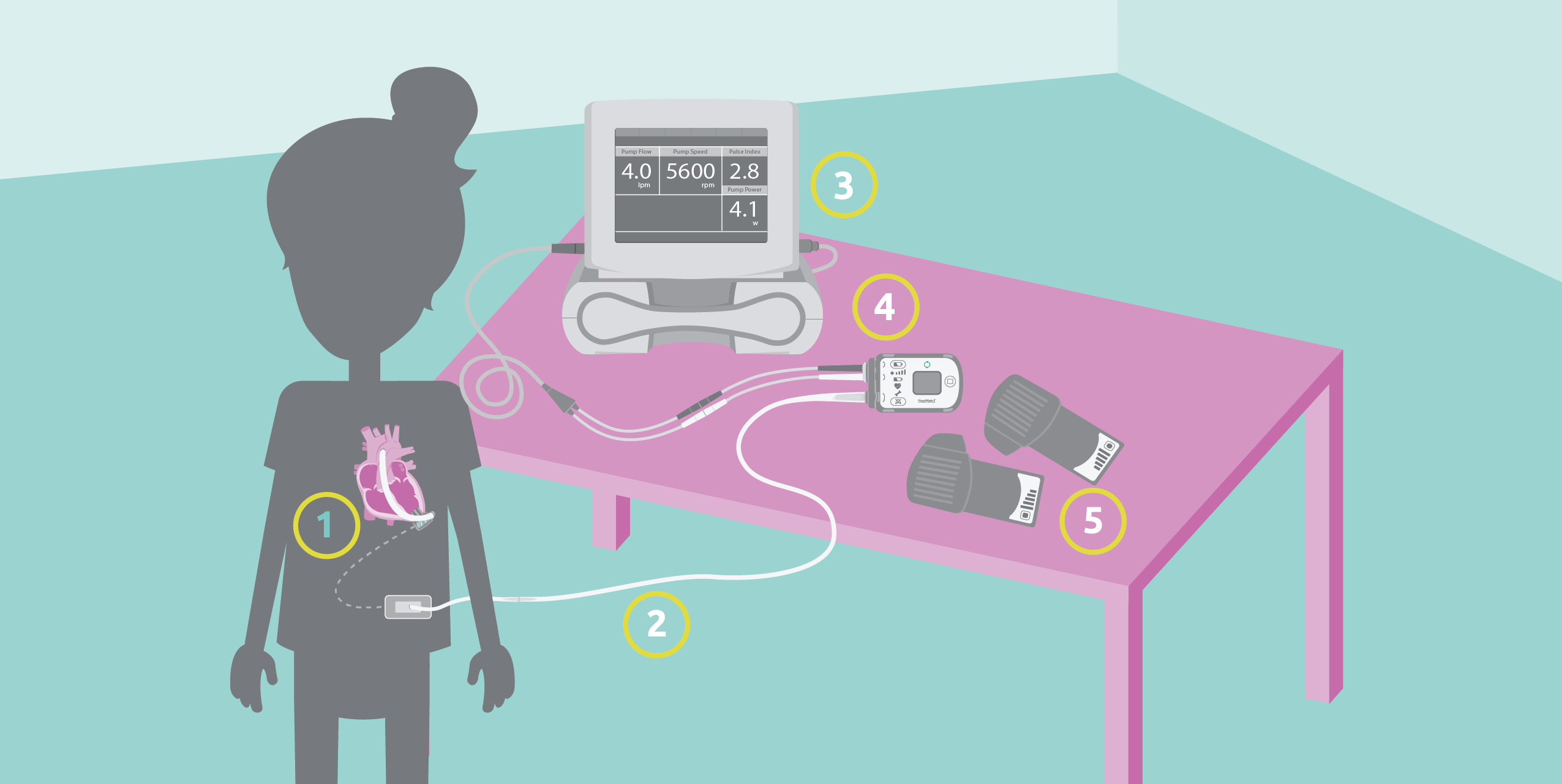
1 VAD
The HeartMate 3™ LVAD is placed inside your chest. The outflow graft is a flexible tube that connects the outflow of the HeartMate 3™ LVAD to the aorta. It helps carry the blood from the pump to the rest of the body. The inside of the pump has a rotor that spins continuously and can distribute up to 10 liters of blood per minute (L/min). 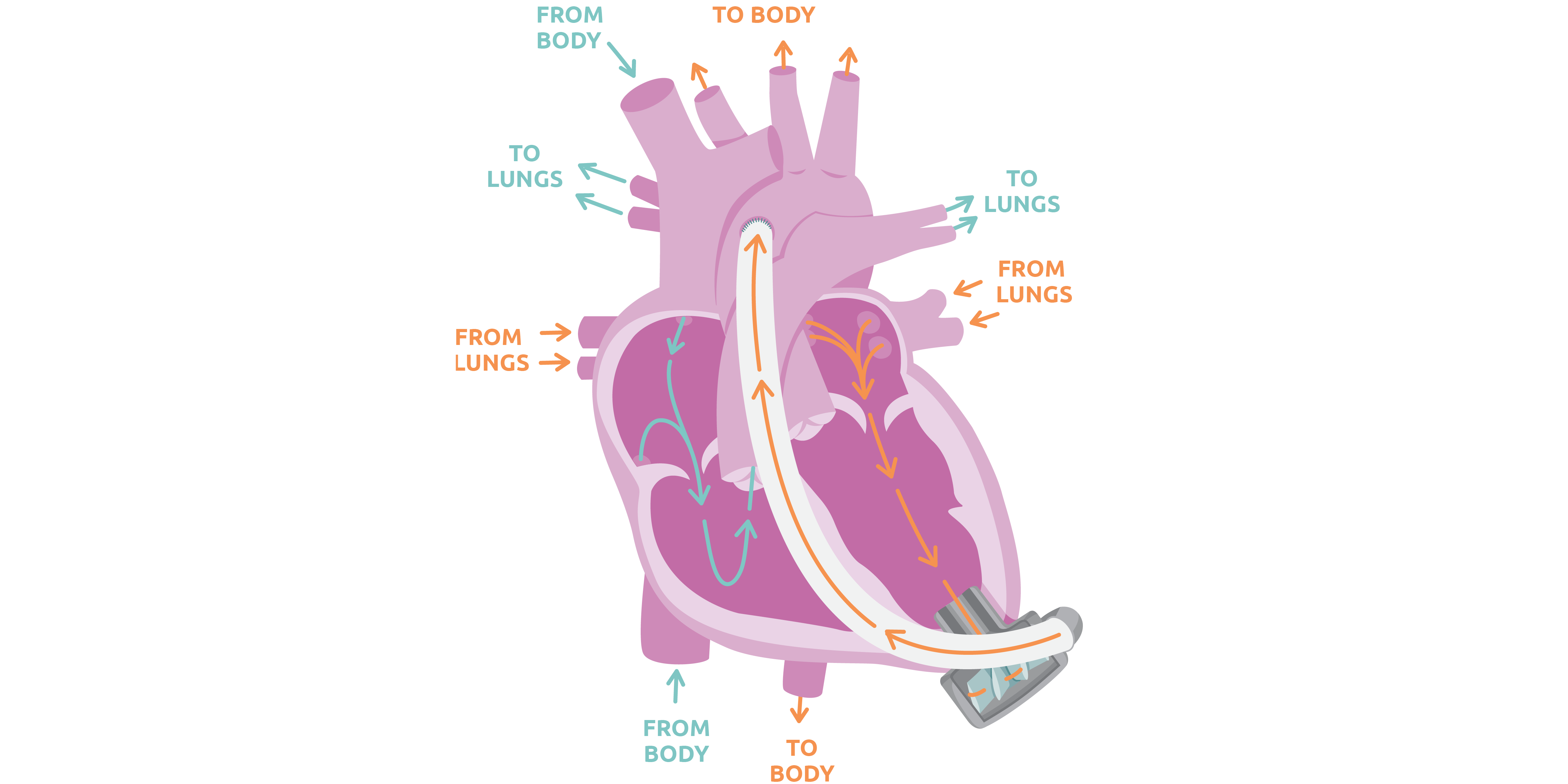
2 Driveline
3 System Monitor
4 System Controller

There are many numbers that you will want to know about. The RPM, or rotations per minute, is set by your care team. The other numbers are calculated but will tell the team a lot about how you are doing. Watch the interactive below to learn more.5 Electrical Power
Benefits
 HeartMate 3™ LVAD can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
HeartMate 3™ LVAD can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
A HeartMate 3™ LVAD may help reduce heart failure symptoms and improve quality of life as you continue along your journey. Is this VAD Right for Me?
Risks

Infection
Stroke
Bleeding
Pediatric VAD Infections
Take ACTION Reducing Stroke Rates
Your Surgery Journey

Preparing
for SurgeryAfter Surgery
Recovery Self Care
Daily Life and Safety
Discharge
Preparing for Surgery
Your Surgery Day
The surgery can take an entire day. The surgeon performs a sternotomy, which involves opening your chest and implanting the VAD device into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation. Explore this interactive to learn more about the surgery.After Surgery


The Cardiac Step-Down Unit, or cardiac floor, is where you may be transferred after the ICU. This floor is for patients who are not as critically ill but still need to be in the hospital. On the cardiac floor, you will focus on getting stronger. During this time, education will become even more important so that you can be discharged from the hospital. However, in some cases, this is not possible. Your care team will discuss this with you.Recovery Self Care
What labs could you need?
What tests could you need?
 Regular testing will become a part of normal life.
Regular testing will become a part of normal life.
What medicines could you take?
When you are on a VAD, you will always be on blood thinner (anticoagulation) medicines. Your care team will increase and decrease the medicines based on your lab results.
You will take aspirin to prevent platelets from sticking together and forming a clot in your VAD.
Warfarin is the most important medicine you will take, but it can be difficult to get your dose (the amount you take) correct. The dose needed will go up and down frequently depending on your INR. Warfarin is what makes your INR (blood levels for anticoagulation or how thick or thin your blood is) increase. In can be tricky because it interacts with lots of different medicines and foods. Your INR can change dramatically with your diet. Warfarin blocks the ability for the body to activate Vitamin K, which helps your body produce blood clots. Green leafy vegetables are rich in vitamin K. Eating lots of these types of foods can decrease your INR or make your blood thicker. It is important to have a consistent diet that includes serving of foods that contain similar amounts of vitamin K each week. Eating a consistent healthy diet will help keep your INR levels on target.
Eating a consistent healthy diet will help keep your INR levels on target.
At times, with a VAD you may have high blood pressure and require medicines to keep the VAD pumping well and can decrease your risk of stroke.
Antibiotics are given in the operating room and ICU to prevent infection. They are also given if your driveline gets infected. Antibiotics can make your INR high or low. Immediately notify your care team if you start taking an antibiotic.
Medicines to prevent “heartburn” are used to decrease the acid in the stomach. This may help with decreasing any stomach discomfort you may have.
Diuretics were important when you were in heart failure. When you are on a VAD you should need less, but you still may need a small amount to get the fluids in your body just right. What complications could occur?
When on blood thinners, you are always at risk of bleeding. You may experience bleeding from your gums when brushing your teeth and your cuts may bleed more than normal. Girls may experience heavier bleeding during menstrual periods and may need to seek additional treatment. If you are involved in a traumatic accident, such as a car accident, it can be harder to stop the bleeding.
To prevent nose bleeds, use petroleum jelly or saline nose spray in your nasal passages during cold, dry weather. Do not pick your nose as this may start a nosebleed. If you have a nose bleed:
Learn more about the risks and signs of bleeding in your belly in the interactive below.
With all VADs there is a risk of stroke, which is caused by bleeding or a blood clot in your brain. Both may cause injury to your brain. Your care team manages your medicines carefully to prevent strokes, however sometimes strokes may occur. Notify your care team or call 911 if you have any of the following symptoms:
Red blood cells help carry oxygen to your tissues and organs. When red blood cells get broken down, this is called hemolysis. Hemolysis may occur for multiple reasons, the most concerning being a mechanical problem with the VAD. Notify your care team if you have any of the following symptoms:
Rarely will the VAD develop a clot inside of it and not work properly. If this happens, and changes to your blood thinner medicine doesn’t fix the problem, you may need to get a new VAD. 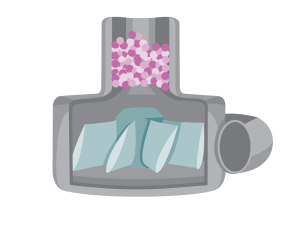 VAD pump clot
VAD pump clot
What should you know about your blood pressure?
How do you care for your driveline site?
Your driveline site will need to have dressing changes using a sterile technique. Everyone should use sterile gloves and wear masks during dressing changes. How often you change your dressings will be determined by your care team.What should you be eating and drinking?
If you have fluid-overload, you may experience:
Learn more about why it’s important to stay hydrated in the interactive below. 
How are you feeling?
Daily Life and Safety
What to pack in your VAD “Go Bag”?
You must always have back up equipment with you in case something happens to one of your VAD components. The following items should be with you at all times:

What to know about travel?
 Take caution when traveling and always carry your VAD emergency information.
Take caution when traveling and always carry your VAD emergency information.
Every state has different rules about driving with a VAD. If you are a licensed driver, use caution within the first 90 days after surgery because you may still be taking medication that may affect your concentration. Some medications will cause side effects that you won’t have adjusted to yet. When you start driving again, take short supervised trips to get used to driving with the new equipment. If you feel dizzy, short of breath, or have blurred vision, pull over to the side of the road immediately and call for help.
You will be able to travel, even on a plane, but it takes some extra planning with your care team to make sure you’re safe. You will need a travel plan and an emergency action plan for long-distance trips. Your care team will make this plan and contact other ACTION hospitals to discuss your care. When traveling by plane, you will NOT go through standard security. You will need to tell the airline agents you have a medical device and they will take you through a separate security lane.What should you know about going back to school or work?

Is exercise right for you?

Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.What do you do when you get a cold?
When you have a VAD, you can still get common colds or other infections unrelated to the VAD. It’s important to have a flu shot every year. And, you should always let your care team know if you are sick. They may direct you to your primary care doctor or have you come into the VAD clinic. Learn about VAD-related infections and inflammation in the interactive below.
What over-the-counter medicines can you take?
When you’re on a VAD, you will sometimes have pain, especially after your surgery.

 Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!
Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!Discharge
 As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged.
As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged.
When should you call your care team?
 Make sure to keep your care team up-to-date with any changes
Make sure to keep your care team up-to-date with any changes Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!
Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!What should I tell my local emergency services? (Medical Services/Fire/Utilities)
 Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Always carry your medical safety card with you in case of an emergency. If you don’t have a medical safety card, download and fill out the ACTION VAD Emergency Medical Safety Card below. Preparing for Surgery
Your Surgery Day
The surgery can take an entire day. The surgeon performs a sternotomy, which involves opening your chest and implanting the VAD device into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation. Explore this interactive to learn more about the surgery.After Surgery


The Cardiac Step-Down Unit, or cardiac floor, is where you may be transferred after the ICU. This floor is for patients who are not as critically ill but still need to be in the hospital. On the cardiac floor, you will focus on getting stronger. During this time, education will become even more important so that you can be discharged from the hospital. However, in some cases, this is not possible. Your care team will discuss this with you.Recovery Self Care
What labs could you need?
What tests could you need?
 Regular testing will become a part of normal life.
Regular testing will become a part of normal life.
What medicines could you take?
When you are on a VAD, you will always be on blood thinner (anticoagulation) medicines. Your care team will increase and decrease the medicines based on your lab results.
You will take aspirin to prevent platelets from sticking together and forming a clot in your VAD.
Warfarin is the most important medicine you will take, but it can be difficult to get your dose (the amount you take) correct. The dose needed will go up and down frequently depending on your INR. Warfarin is what makes your INR (blood levels for anticoagulation or how thick or thin your blood is) increase. In can be tricky because it interacts with lots of different medicines and foods. Your INR can change dramatically with your diet. Warfarin blocks the ability for the body to activate Vitamin K, which helps your body produce blood clots. Green leafy vegetables are rich in vitamin K. Eating lots of these types of foods can decrease your INR or make your blood thicker. It is important to have a consistent diet that includes serving of foods that contain similar amounts of vitamin K each week. Eating a consistent healthy diet will help keep your INR levels on target.
Eating a consistent healthy diet will help keep your INR levels on target.
At times, with a VAD you may have high blood pressure and require medicines to keep the VAD pumping well and can decrease your risk of stroke.
Antibiotics are given in the operating room and ICU to prevent infection. They are also given if your driveline gets infected. Antibiotics can make your INR high or low. Immediately notify your care team if you start taking an antibiotic.
Medicines to prevent “heartburn” are used to decrease the acid in the stomach. This may help with decreasing any stomach discomfort you may have.
Diuretics were important when you were in heart failure. When you are on a VAD you should need less, but you still may need a small amount to get the fluids in your body just right. What complications could occur?
When on blood thinners, you are always at risk of bleeding. You may experience bleeding from your gums when brushing your teeth and your cuts may bleed more than normal. Girls may experience heavier bleeding during menstrual periods and may need to seek additional treatment. If you are involved in a traumatic accident, such as a car accident, it can be harder to stop the bleeding.
To prevent nose bleeds, use petroleum jelly or saline nose spray in your nasal passages during cold, dry weather. Do not pick your nose as this may start a nosebleed. If you have a nose bleed:
Learn more about the risks and signs of bleeding in your belly in the interactive below.
With all VADs there is a risk of stroke, which is caused by bleeding or a blood clot in your brain. Both may cause injury to your brain. Your care team manages your medicines carefully to prevent strokes, however sometimes strokes may occur. Notify your care team or call 911 if you have any of the following symptoms:
Red blood cells help carry oxygen to your tissues and organs. When red blood cells get broken down, this is called hemolysis. Hemolysis may occur for multiple reasons, the most concerning being a mechanical problem with the VAD. Notify your care team if you have any of the following symptoms:
Rarely will the VAD develop a clot inside of it and not work properly. If this happens, and changes to your blood thinner medicine doesn’t fix the problem, you may need to get a new VAD. 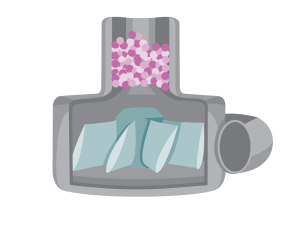 VAD pump clot
VAD pump clot
What should you know about your blood pressure?
How do you care for your driveline site?
Your driveline site will need to have dressing changes using a sterile technique. Everyone should use sterile gloves and wear masks during dressing changes. How often you change your dressings will be determined by your care team.What should you be eating and drinking?
If you have fluid-overload, you may experience:
Learn more about why it’s important to stay hydrated in the interactive below. 
How are you feeling?
Daily Life and Safety
What to pack in your VAD “Go Bag”?
You must always have back up equipment with you in case something happens to one of your VAD components. The following items should be with you at all times:

What to know about travel?
 Take caution when traveling and always carry your VAD emergency information.
Take caution when traveling and always carry your VAD emergency information.
Every state has different rules about driving with a VAD. If you are a licensed driver, use caution within the first 90 days after surgery because you may still be taking medication that may affect your concentration. Some medications will cause side effects that you won’t have adjusted to yet. When you start driving again, take short supervised trips to get used to driving with the new equipment. If you feel dizzy, short of breath, or have blurred vision, pull over to the side of the road immediately and call for help.
You will be able to travel, even on a plane, but it takes some extra planning with your care team to make sure you’re safe. You will need a travel plan and an emergency action plan for long-distance trips. Your care team will make this plan and contact other ACTION hospitals to discuss your care. When traveling by plane, you will NOT go through standard security. You will need to tell the airline agents you have a medical device and they will take you through a separate security lane.What should you know about going back to school or work?

Is exercise right for you?

Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.What do you do when you get a cold?
When you have a VAD, you can still get common colds or other infections unrelated to the VAD. It’s important to have a flu shot every year. And, you should always let your care team know if you are sick. They may direct you to your primary care doctor or have you come into the VAD clinic. Learn about VAD-related infections and inflammation in the interactive below.
What over-the-counter medicines can you take?
When you’re on a VAD, you will sometimes have pain, especially after your surgery.

 Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!
Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!Discharge
 As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged.
As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged.
When should you call your care team?
 Make sure to keep your care team up-to-date with any changes
Make sure to keep your care team up-to-date with any changes Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!
Download our VAD-Venture iOS App for the HeartMate 3™ LVAD!What should I tell my local emergency services? (Medical Services/Fire/Utilities)
 Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Always carry your medical safety card with you in case of an emergency. If you don’t have a medical safety card, download and fill out the ACTION VAD Emergency Medical Safety Card below. HVAD™ System
Notice to all Patients, Families, & Care Givers
Overview
Your Surgery Journey
Overview
Device Components
Benefits
Risks
Device Components

1 HVAD
The HVAD is implanted inside of your chest. The outflow graft is a flexible tube that connects the outflow of the pump to the aorta. It helps carry the blood from the pump to the rest of the body. The inside of the pump has an impeller that spins continuously and can distribute up to 10 liters of blood per minute (L/min). 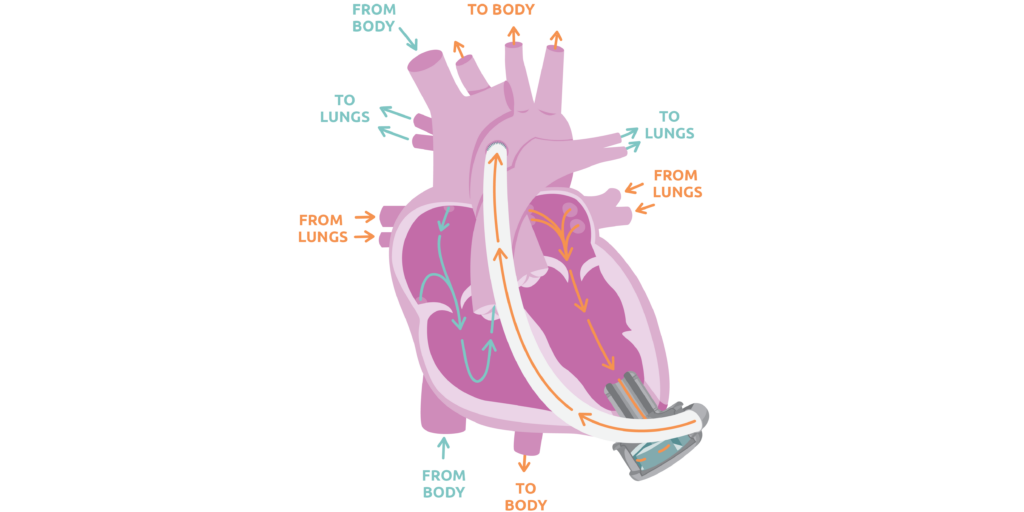
2 Driveline
3 Monitor
4 Controller

There are many numbers that you will want to know about. The RPM, or rotations per minute, is set by your care team. The other numbers are calculated but will tell the team a lot about how you are doing.Electrical Power
Benefits

Is this VAD Right for Me?
Risks

Infection
Stroke
Bleeding
Pediatric VAD Infections
Take ACTION Reducing Stroke Rates
Device Components

1 HVAD
The HVAD is implanted inside of your chest. The outflow graft is a flexible tube that connects the outflow of the pump to the aorta. It helps carry the blood from the pump to the rest of the body. The inside of the pump has an impeller that spins continuously and can distribute up to 10 liters of blood per minute (L/min). 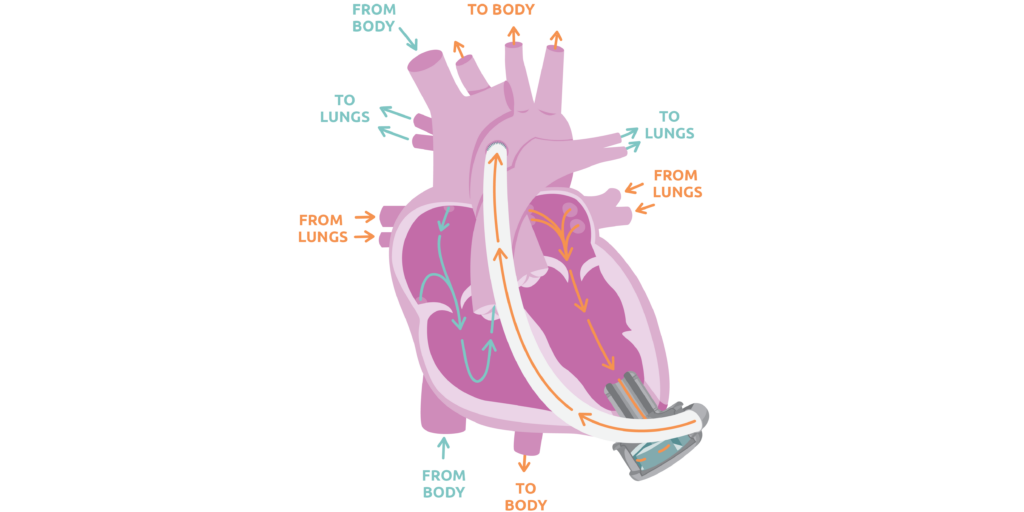
2 Driveline
3 Monitor
4 Controller

There are many numbers that you will want to know about. The RPM, or rotations per minute, is set by your care team. The other numbers are calculated but will tell the team a lot about how you are doing.Electrical Power
Benefits

Is this VAD Right for Me?
Risks

Infection
Stroke
Bleeding
Pediatric VAD Infections
Take ACTION Reducing Stroke Rates
Your Surgery Journey

Preparing
for SurgeryAfter Surgery
Recovery Self Care
Daily Life
and SafetyDischarge
Preparing for Surgery
Your Surgery Day
The surgery can take an entire day. The surgeon performs a sternotomy, which involves opening your chest and implanting the HVAD™ System device into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation.After Surgery


The Cardiac Step-Down Unit, or cardiac floor, is where you may be transferred after the ICU. This floor is for patients who are not as critically ill but still need to be in the hospital. On the cardiac floor, you will focus on getting stronger. During this time, education will become even more important so that you can be discharged from the hospital. However, in some cases, this is not possible. Your care team will discuss this with you.Recovery Self Care
What labs could you need?
What tests could you need?
 Regular testing will become a part of normal life.
Regular testing will become a part of normal life.
What medicines could you take?
In the hospital, medicine will be given through an IV. Your care team will change those medicines to be given by mouth when preparing for discharge. It’s important the medicines are taken at the same time every day. By the time you are ready to go home, medicines will likely be taken twice a day. Use a pill box to keep your medicines organized. Inform your care team if you take any additional medicines NOT prescribed by them. Learn more about medicines through the interactive below.
Blood Thinning Medicines
When you are on a VAD, you will always be on blood thinner (anticoagulation) medicines. Your care team will increase and decrease the medicines based on your lab results.
You will take aspirin to prevent platelets from sticking together and forming a clot in your VAD.
Warfarin is the most important medicine you will take, but it can be difficult to get your dose (the amount you take) correct. The dose needed will go up and down frequently depending on your INR. Warfarin is what makes your INR (blood levels for anticoagulation or how thick or thin your blood is) increase. In can be tricky because it interacts with lots of different medicines and foods. Your INR can change dramatically with your diet. Warfarin blocks the ability for the body to activate Vitamin K, which helps your body produce blood clots. Green leafy vegetables are rich in vitamin K. Eating lots of these types of foods can decrease your INR or make your blood thicker. It is important to have a consistent diet that includes serving of foods that contain similar amounts of vitamin K each week. Eating a consistent healthy diet will help keep your INR levels on target.
Eating a consistent healthy diet will help keep your INR levels on target.
At times, with a VAD you may have high blood pressure and require medicines to keep the VAD pumping well and can decrease your risk of stroke.
Antibiotics are given in the operating room and ICU to prevent infection. They are also given if your driveline gets infected. Antibiotics can make your INR high or low. Immediately notify your care team if you start taking an antibiotic.
Medicines to prevent “heartburn” are used to decrease the acid in the stomach. This may help with decreasing any stomach discomfort you may have.
Diuretics were important when you were in heart failure. When you are on a VAD you should need less, but you still may need a small amount to get the fluids in your body just right. What complications could occur?
When on blood thinners, you are always at risk of bleeding. You may experience bleeding from your gums when brushing your teeth and your cuts may bleed more than normal. Girls may experience heavier bleeding during menstrual periods and may need to seek additional treatment. If you are involved in a traumatic accident, such as a car accident, it can be harder to stop the bleeding.
To prevent nose bleeds, use petroleum jelly or saline nose spray in your nasal passages during cold, dry weather. Do not pick your nose as this may start a nosebleed. If you have a nose bleed:
Learn more about the risks and signs of bleeding in your belly in the interactive below.
With all VADs there is a risk of stroke, which is caused by bleeding or a blood clot in your brain. Both may cause injury to your brain. Your care team manages your medicines carefully to prevent strokes, however sometimes strokes may occur. Notify your care team or call 911 if you have any of the following symptoms:
Red blood cells help carry oxygen to your tissues and organs. When red blood cells get broken down, this is called hemolysis. Hemolysis may occur for multiple reasons, the most concerning being a mechanical problem with the VAD. Notify your care team if you have any of the following symptoms:
Rarely will the VAD develop a clot inside of it and not work properly. If this happens, and changes to your blood thinner medicine doesn’t fix the problem, you may need to get a new VAD. 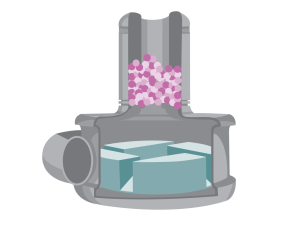 HVAD pump clot
HVAD pump clot
What should you know about your blood pressure?
How do you care for your driveline site?
Your driveline site will need to have dressing changes using a sterile technique. Everyone should use sterile gloves and wear masks during dressing changes. How often you change your dressings will be determined by your care team.What should you be eating and drinking?
If you have fluid-overload, you may experience:
Learn more about why it’s important to stay hydrated in the interactive below. 
How are you feeling?
Daily Life and Safety
What to pack in your VAD “Go Bag”?

What to know about travel?
 Take caution when traveling and always carry your VAD emergency information.
Take caution when traveling and always carry your VAD emergency information.
Every state has different rules about driving with a VAD. If you are a licensed driver, use caution within the first 90 days after surgery because you may still be taking medication that may affect your concentration. Some medications will cause side effects that you won’t have adjusted to yet. When you start driving again, take short supervised trips to get used to driving with the new equipment. If you feel dizzy, short of breath, or have blurred vision, pull over to the side of the road immediately and call for help.
You will be able to travel, even on a plane, but it takes some extra planning with your care team to make sure you’re safe. You will need a travel plan and an emergency action plan for long-distance trips. Your care team will make this plan and contact other ACTION hospitals to discuss your care. When traveling by plane, you will NOT go through standard security. You will need to tell the airline agents you have a medical device and they will take you through a separate security lane.What should you know about going back to school or work?

Is exercise right for you?
 Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.
If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily.
Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.
If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily. What do you do when you get a cold?
When you have a VAD, you can still get common colds or other infections unrelated to the VAD. It’s important to have a flu shot every year. And, you should always let your care team know if you are sick. They may direct you to your primary care doctor or have you come into the VAD clinic. Learn about VAD-related infections and inflammation in the interactive below.
What over-the-counter medicines can you take?
When you’re on a VAD, you will sometimes have pain, especially after your surgery.

Discharge
 As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged
As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be dischargedWhen should you call your care team?
 Make sure to keep your care team up-to-date with any changes
Make sure to keep your care team up-to-date with any changesWhat should I tell my local emergency services? (Medical Services/Fire/Utilities)
 Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Always carry your medical safety card with you in case of an emergency. If you don’t have a medical safety card, download and fill out the ACTION VAD Emergency Medical Safety Card below. Preparing for Surgery
Your Surgery Day
The surgery can take an entire day. The surgeon performs a sternotomy, which involves opening your chest and implanting the HVAD™ System device into your heart. This will leave a scar on your chest. During the surgery, you will be on a heart and lung bypass machine, which helps circulate your blood during the operation.After Surgery


The Cardiac Step-Down Unit, or cardiac floor, is where you may be transferred after the ICU. This floor is for patients who are not as critically ill but still need to be in the hospital. On the cardiac floor, you will focus on getting stronger. During this time, education will become even more important so that you can be discharged from the hospital. However, in some cases, this is not possible. Your care team will discuss this with you.Recovery Self Care
What labs could you need?
What tests could you need?
 Regular testing will become a part of normal life.
Regular testing will become a part of normal life.
What medicines could you take?
In the hospital, medicine will be given through an IV. Your care team will change those medicines to be given by mouth when preparing for discharge. It’s important the medicines are taken at the same time every day. By the time you are ready to go home, medicines will likely be taken twice a day. Use a pill box to keep your medicines organized. Inform your care team if you take any additional medicines NOT prescribed by them. Learn more about medicines through the interactive below.
Blood Thinning Medicines
When you are on a VAD, you will always be on blood thinner (anticoagulation) medicines. Your care team will increase and decrease the medicines based on your lab results.
You will take aspirin to prevent platelets from sticking together and forming a clot in your VAD.
Warfarin is the most important medicine you will take, but it can be difficult to get your dose (the amount you take) correct. The dose needed will go up and down frequently depending on your INR. Warfarin is what makes your INR (blood levels for anticoagulation or how thick or thin your blood is) increase. In can be tricky because it interacts with lots of different medicines and foods. Your INR can change dramatically with your diet. Warfarin blocks the ability for the body to activate Vitamin K, which helps your body produce blood clots. Green leafy vegetables are rich in vitamin K. Eating lots of these types of foods can decrease your INR or make your blood thicker. It is important to have a consistent diet that includes serving of foods that contain similar amounts of vitamin K each week. Eating a consistent healthy diet will help keep your INR levels on target.
Eating a consistent healthy diet will help keep your INR levels on target.
At times, with a VAD you may have high blood pressure and require medicines to keep the VAD pumping well and can decrease your risk of stroke.
Antibiotics are given in the operating room and ICU to prevent infection. They are also given if your driveline gets infected. Antibiotics can make your INR high or low. Immediately notify your care team if you start taking an antibiotic.
Medicines to prevent “heartburn” are used to decrease the acid in the stomach. This may help with decreasing any stomach discomfort you may have.
Diuretics were important when you were in heart failure. When you are on a VAD you should need less, but you still may need a small amount to get the fluids in your body just right. What complications could occur?
When on blood thinners, you are always at risk of bleeding. You may experience bleeding from your gums when brushing your teeth and your cuts may bleed more than normal. Girls may experience heavier bleeding during menstrual periods and may need to seek additional treatment. If you are involved in a traumatic accident, such as a car accident, it can be harder to stop the bleeding.
To prevent nose bleeds, use petroleum jelly or saline nose spray in your nasal passages during cold, dry weather. Do not pick your nose as this may start a nosebleed. If you have a nose bleed:
Learn more about the risks and signs of bleeding in your belly in the interactive below.
With all VADs there is a risk of stroke, which is caused by bleeding or a blood clot in your brain. Both may cause injury to your brain. Your care team manages your medicines carefully to prevent strokes, however sometimes strokes may occur. Notify your care team or call 911 if you have any of the following symptoms:
Red blood cells help carry oxygen to your tissues and organs. When red blood cells get broken down, this is called hemolysis. Hemolysis may occur for multiple reasons, the most concerning being a mechanical problem with the VAD. Notify your care team if you have any of the following symptoms:
Rarely will the VAD develop a clot inside of it and not work properly. If this happens, and changes to your blood thinner medicine doesn’t fix the problem, you may need to get a new VAD.  HVAD pump clot
HVAD pump clot
What should you know about your blood pressure?
How do you care for your driveline site?
Your driveline site will need to have dressing changes using a sterile technique. Everyone should use sterile gloves and wear masks during dressing changes. How often you change your dressings will be determined by your care team.What should you be eating and drinking?
If you have fluid-overload, you may experience:
Learn more about why it’s important to stay hydrated in the interactive below. 
How are you feeling?
Daily Life and Safety
What to pack in your VAD “Go Bag”?

What to know about travel?
 Take caution when traveling and always carry your VAD emergency information.
Take caution when traveling and always carry your VAD emergency information.
Every state has different rules about driving with a VAD. If you are a licensed driver, use caution within the first 90 days after surgery because you may still be taking medication that may affect your concentration. Some medications will cause side effects that you won’t have adjusted to yet. When you start driving again, take short supervised trips to get used to driving with the new equipment. If you feel dizzy, short of breath, or have blurred vision, pull over to the side of the road immediately and call for help.
You will be able to travel, even on a plane, but it takes some extra planning with your care team to make sure you’re safe. You will need a travel plan and an emergency action plan for long-distance trips. Your care team will make this plan and contact other ACTION hospitals to discuss your care. When traveling by plane, you will NOT go through standard security. You will need to tell the airline agents you have a medical device and they will take you through a separate security lane.What should you know about going back to school or work?

Is exercise right for you?
 Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.
If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily.
Once you’ve recovered from surgery you should be exercising to get stronger. You may be instructed to do special exercises at home or you may be asked to come to the hospital frequently to exercise in the clinic. Your care team will help you choose exercises that you can do safely.
If you have a wearable tracking device, talk to your care team about coming up with a step goal to keep you moving daily. What do you do when you get a cold?
When you have a VAD, you can still get common colds or other infections unrelated to the VAD. It’s important to have a flu shot every year. And, you should always let your care team know if you are sick. They may direct you to your primary care doctor or have you come into the VAD clinic. Learn about VAD-related infections and inflammation in the interactive below.
What over-the-counter medicines can you take?
When you’re on a VAD, you will sometimes have pain, especially after your surgery.

Discharge
 As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be discharged
As you recover from your surgery, there may be a period of time when you are required to stay near the hospital and have frequent clinic visits. Once the care team feels it’s safe for you to return home and go to school or work, multiple steps will occur to ensure your safety. Your care team will explain the specific accomplishments you must achieve in order to be dischargedWhen should you call your care team?
 Make sure to keep your care team up-to-date with any changes
Make sure to keep your care team up-to-date with any changesWhat should I tell my local emergency services? (Medical Services/Fire/Utilities)
 Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Either you or your care team members should notify your local emergency medical department when you are discharged. It is nice for them to know you are at home with life-saving equipment. If you lose electricity, you must relocate to a new location. You can contact your care team if you have questions about what to do.
Always carry your medical safety card with you in case of an emergency. If you don’t have a medical safety card, download and fill out the ACTION VAD Emergency Medical Safety Card below. PediMag™ & CentriMag™
Overview
Your Surgery Journey
Overview
Device Components
Benefits
Risks
Device Components
Cannula
Circuit
Blood Pump
Console
Benefits
 CentriMag™ and PediMag™ can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
CentriMag™ and PediMag™ can be used to help a heart pump for many reasons. Depending on your situation, it may be used as: Risks
 There are also some risks associated with having a VAD, but your care team will work hard to keep you safe.
There are also some risks associated with having a VAD, but your care team will work hard to keep you safe.Infection
Bleeding
Stroke
Pediatric VAD Infections
Take ACTION Reducing Stroke Rates
Device Components
Cannula
Circuit
Blood Pump
Console
Benefits
 CentriMag™ and PediMag™ can be used to help a heart pump for many reasons. Depending on your situation, it may be used as:
CentriMag™ and PediMag™ can be used to help a heart pump for many reasons. Depending on your situation, it may be used as: Risks
 There are also some risks associated with having a VAD, but your care team will work hard to keep you safe.
There are also some risks associated with having a VAD, but your care team will work hard to keep you safe.Infection
Bleeding
Stroke
Pediatric VAD Infections
Take ACTION Reducing Stroke Rates
Your Surgery Journey

Preparing
for SurgeryAfter Surgery
Recovery
Preparing for Surgery
 Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.
Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.Your Surgery Day
After Surgery
 When you wake up from surgery, you will be in the Intensive Care Unit (ICU).
When you wake up from surgery, you will be in the Intensive Care Unit (ICU).Recovery Self Care
Preparing for Surgery
 Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.
Throughout your journey, your care team is there to support and guide you, as well as answer any questions or concerns you have.Your Surgery Day
After Surgery
 When you wake up from surgery, you will be in the Intensive Care Unit (ICU).
When you wake up from surgery, you will be in the Intensive Care Unit (ICU).Recovery Self Care
Being on the heart transplant waitlist is a time to be hopeful about the next phase in your journey. There is also a lot to know. Let’s take a few minutes to watch the video below and learn more about the transplant waiting list process. Families and patients sometimes have to wait years for a heart transplant. ACTION is working to help patients become stronger and healthier while they wait for a life-saving transplant. This work has especially touched the hearts of the McQueen Family and they now help lead our efforts! Watch the video below to learn more. For information about transplants, including a patient and family guidebook please visit their website here. Check out our quick facts guide which includes information about: How long could a transplanted heart last?Overview
Waiting for My New Heart
Additional Resources
Pediatric Heart Transplant Society
10 Things for VAD Patients To Know About Pediatric Heart Transplants
At home you will lay on a special pillow that reads the pressures in your pulmonary artery and sends the readings to your care team electronically. These pressure readings help your care team manage your heart failure symptoms and check for early signs of worsening heart failure. Your care team will call you if your pressure numbers are outside of the range they would like for you. They may need to make changes to your medicines or they may want to see you in person. Want more information? The device is implanted during a cardiac catheterization procedure. Placement does not require an open heart surgery. It has no battery and is designed to remain in place for life. CardioMEMS™ has helped decrease heart failure hospital admissions by almost 50% in adult patients, so it has the potential to decrease your chance of entering the hospital for heart failure treatment. It helps your care team know how the heart is functioning and what medications are needed. CardioMEMS™ can improve your quality of life by: Since your heart pressures are reviewed more often with this device, it may also decrease the need for future cardiac catheterizations. Adverse rates are minimal for CardioMEMS™ placement. The CardioMEMS™ is placed during a cardiac catheterization, so your care team will monitor your insertion site for any bleeding, swelling, or change in color or temperature of your legs. In rare instances, a small blood clot could form at your insertion site and your legs may not get the normal full blood supply to your toes. If this happens, you may have to come back to the hospital for treatment. You will need to be on a blood thinner medicine after the placement of your CardioMEMS™ for a short period of time. This will decrease the risk of additional complications not related to blood clots. CardioMEMS™ has helped decrease heart failure hospital admissions by almost 50% in adult patients, so it has the potential to decrease your chance of entering the hospital for heart failure treatment. It helps your care team know how the heart is functioning and what medications are needed. CardioMEMS™ can improve your quality of life by: Since your heart pressures are reviewed more often with this device, it may also decrease the need for future cardiac catheterizations. Adverse rates are minimal for CardioMEMS™ placement. The CardioMEMS™ is placed during a cardiac catheterization, so your care team will monitor your insertion site for any bleeding, swelling, or change in color or temperature of your legs. In rare instances, a small blood clot could form at your insertion site and your legs may not get the normal full blood supply to your toes. If this happens, you may have to come back to the hospital for treatment. You will need to be on a blood thinner medicine after the placement of your CardioMEMS™ for a short period of time. This will decrease the risk of additional complications not related to blood clots.Overview
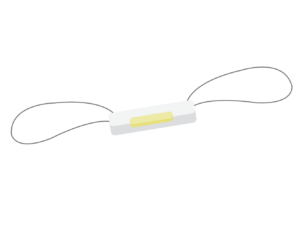 A CardioMEMS™ is an implantable wireless device that sits in the pulmonary artery, a blood vessel that takes blood from your heart to your lungs. The device measures the pressure in your pulmonary artery. The pressure in your pulmonary artery reflects how your heart is squeezing and relaxing, as well as marks how much fluid you have in your body.
A CardioMEMS™ is an implantable wireless device that sits in the pulmonary artery, a blood vessel that takes blood from your heart to your lungs. The device measures the pressure in your pulmonary artery. The pressure in your pulmonary artery reflects how your heart is squeezing and relaxing, as well as marks how much fluid you have in your body.
Check out our CardioMEMs™ HF System patient and family education flyer.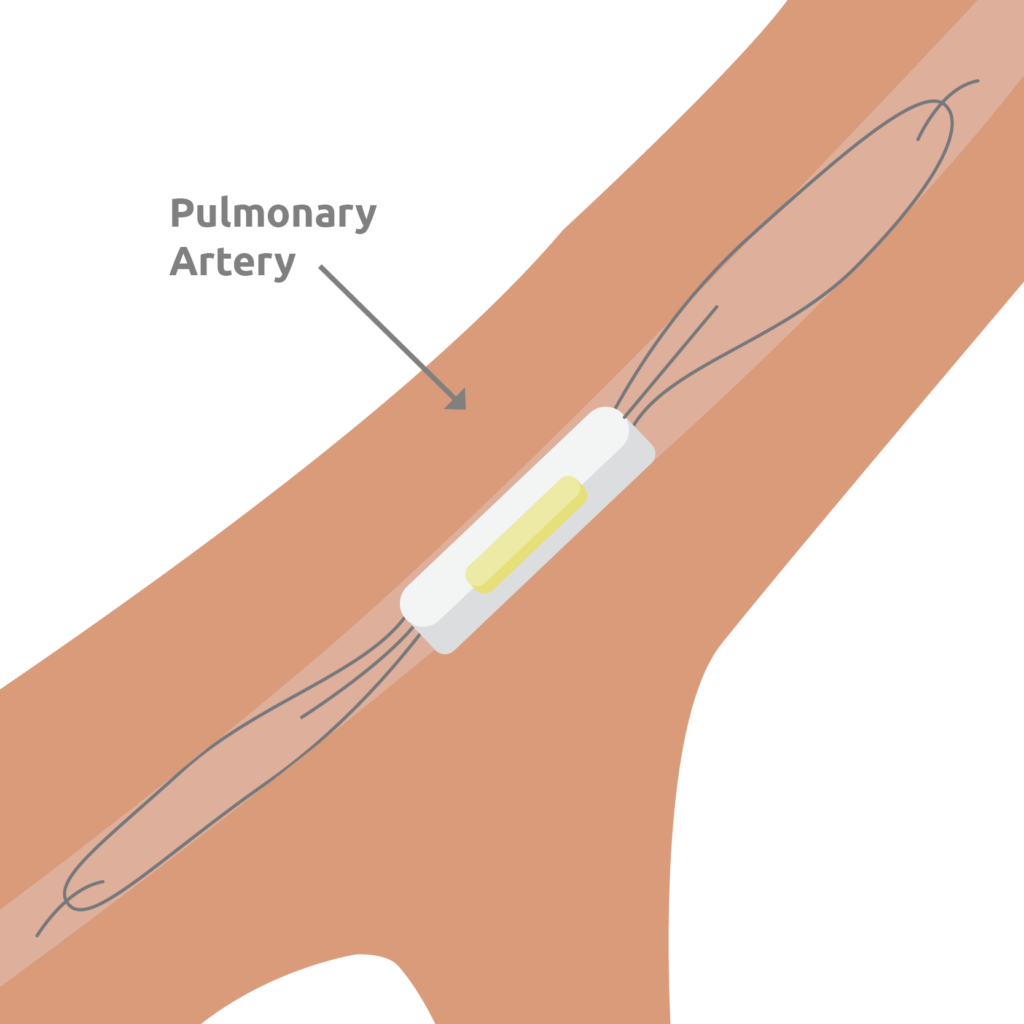
Implanting Your Device
Benefits
Risks
Benefits

Risks






 Math & Mechanics
Math & Mechanics


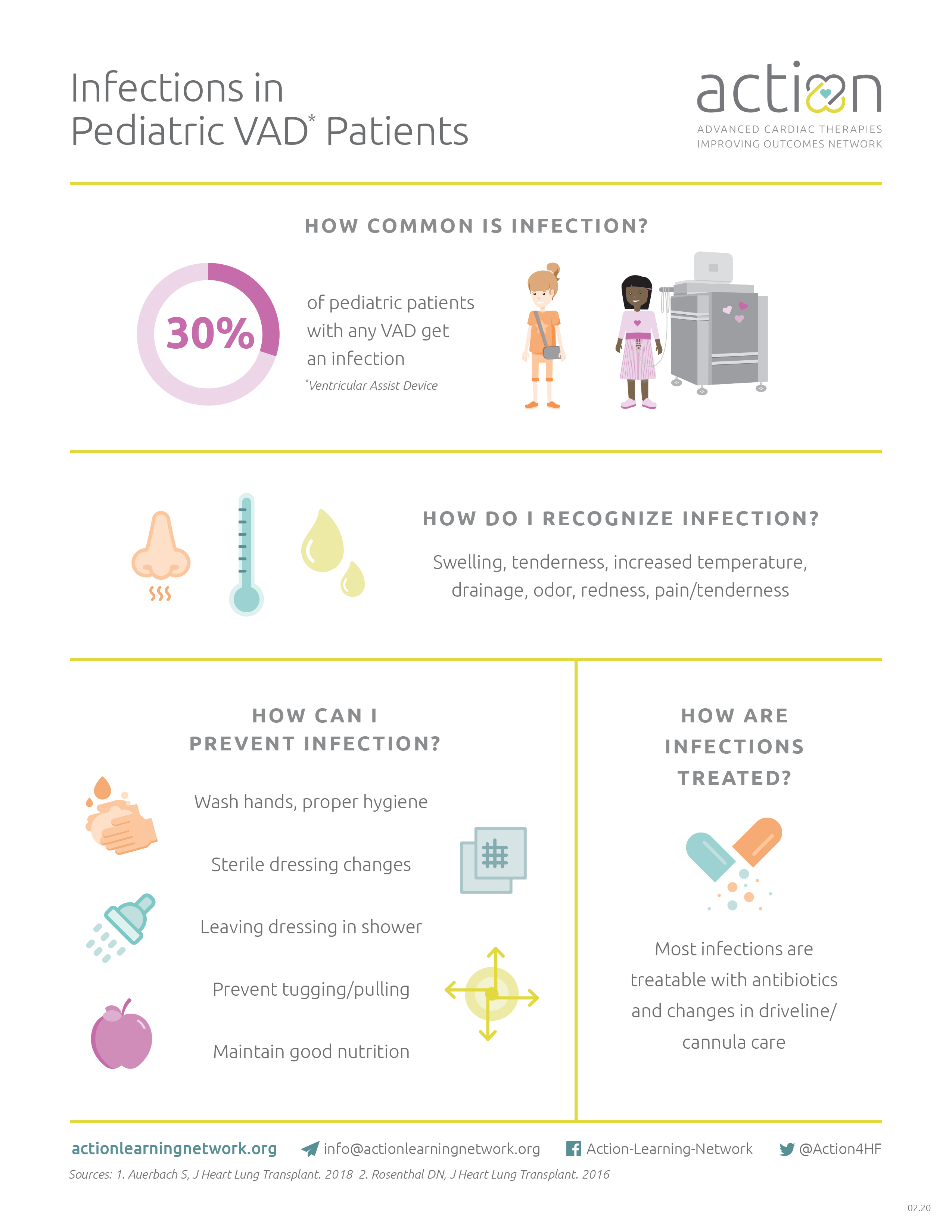


 HeartMate3™ LVAD Patient Journey
HeartMate3™ LVAD Patient Journey
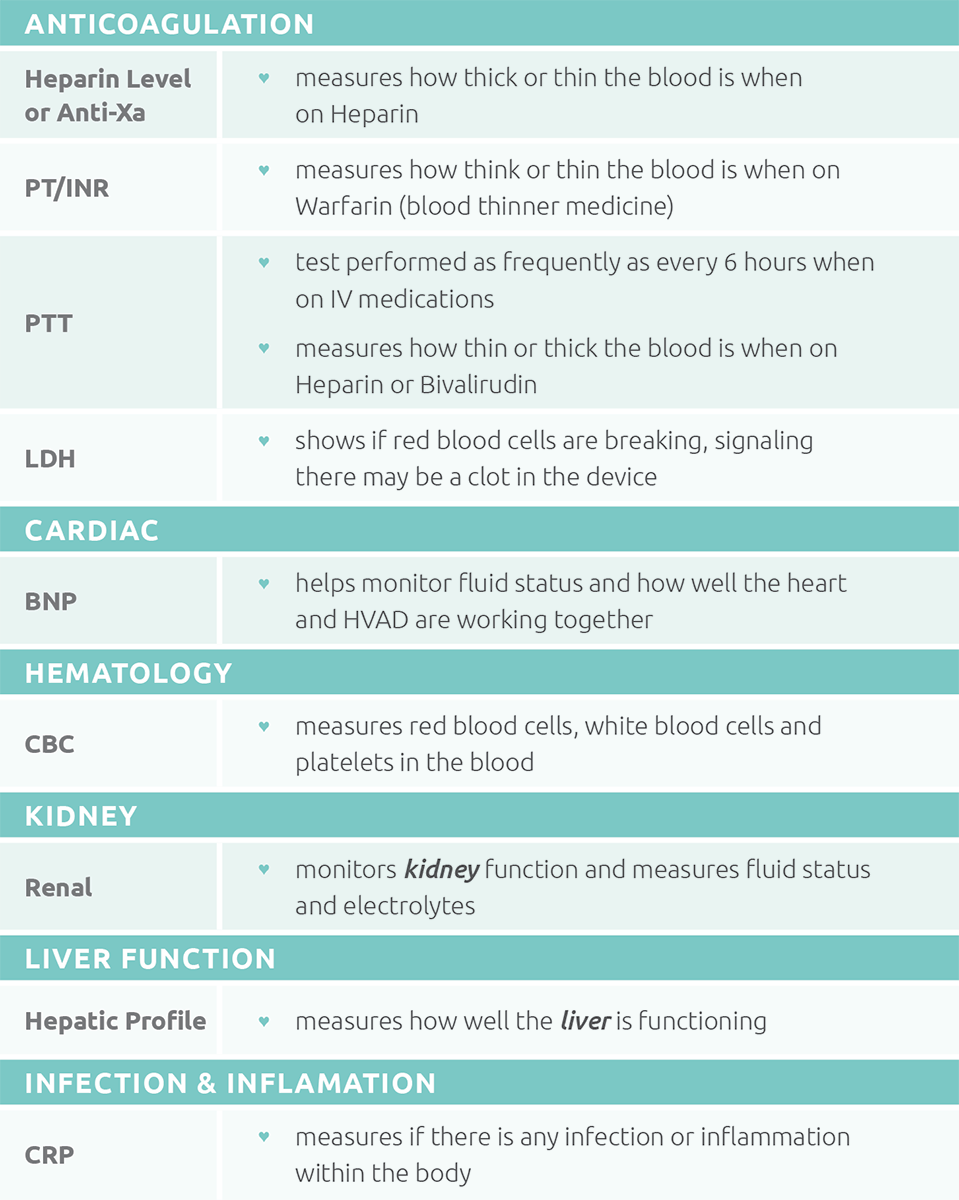

 Take ACTION Reducing Stroke Rates
Take ACTION Reducing Stroke Rates







 Math & Mechanics
Math & Mechanics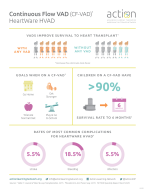
 HVAD™ System Patient Journey
HVAD™ System Patient Journey