Knowing Your Device and
Understanding Surgery
Over the years, advanced technology has been used to develop devices to help patients diagnosed with heart failure. Many of these devices, although designed for adults, have been adapted for use in children. Let’s explore each device and what to expect before, during, and after surgery.
Over the years, advanced technology has been used to develop devices to help patients diagnosed
with heart failure. Many of these devices, although designed for adults, have been adapted for use
in children. Let’s explore each device and what to expect before, during, and after surgery.
-
1
Pacemaker/ICD
-
2
VADs
-
3
Pre-Transplant
-
4
CardioMEMS™
Sometimes patients with heart failure will have abnormal heart rhythms or their doctor feels like they are at increased risk of having a life-threatening heart rhythm. When a heart rhythm isn’t normal (called arrhythmia), it can cause the heart to beat too slowly (bradycardia), too quickly (tachycardia), or abnormally (dysrhythmia). Also, if the pathway is blocked between the upper and lower parts of the heart, the heart may beat at different rates (called a heart block). A pacemaker or automatic implantable cardioverter defibrillator (ICD) can correct the electrical activity and fix abnormal heart rhythms. An arrhythmia can cause symptoms like fluttering in the chest, dizziness, tiredness, or may even cause fainting. Some arrhythmias are life-threatening and may cause the heart to quiver, which prevents blood from getting to the brain and body. This is considered an emergency situation that requires a defibrillator to shock the heart to reset the rhythm immediately. Pacemakers monitor the heart’s rhythm and send a low voltage electrical signal to the heart to “pace” the heart into a correct rhythm. Pacemakers can be used for a short or long amount of time and can be placed internally (inside the body) or externally (outside the body). The short-term external pacemakers are typically used: The long-term internal pacemaker is a small device with wires that lead to the heart chambers. It is implanted into the chest or belly to help the heart beat at a normal rhythm. Pacemakers typically last for many years. Pacemakers deliver low voltage impulses to correct the heart rhythm. However, an ICD detects lethal arrhythmias and delivers high voltage shocks to reset the heart rhythm during a life-threatening emergency. The pacemaker or ICD implant surgery is a minor surgery when placed through a vessel. Often this procedure is done quickly, however times will vary per patient. During the procedure, the surgeon makes an incision into the skin, places the wires inside the heart chambers, and inserts the small device underneath the skin. The pacemaker or ICD is turned on and the settings are adjusted. Afterwards, the incision is closed. There are some restrictions in activity level for a short time after surgery, but normal activity may resume within a few weeks after implant. Benefits of having a Pacemaker/ICD include: Risks related to Pacemaker/ICD surgery include: Benefits of having a Pacemaker/ICD include: Risks related to Pacemaker/ICD surgery include:Overview
 What happens when you turn on a light switch? Electricity travels quickly through wiring that makes a lightbulb glow! The heart works in a similar way. There is a small amount of electricity that moves through a pathway that starts at the top of the heart and travels to the bottom, causing the heart to beat. These electrical signals are called heart rhythms and can be seen when you are connected to an EKG or heart monitor.
What happens when you turn on a light switch? Electricity travels quickly through wiring that makes a lightbulb glow! The heart works in a similar way. There is a small amount of electricity that moves through a pathway that starts at the top of the heart and travels to the bottom, causing the heart to beat. These electrical signals are called heart rhythms and can be seen when you are connected to an EKG or heart monitor.Pacemakers vs ICD

Implanting Your Device
Benefits
Risks
Benefits

Risks



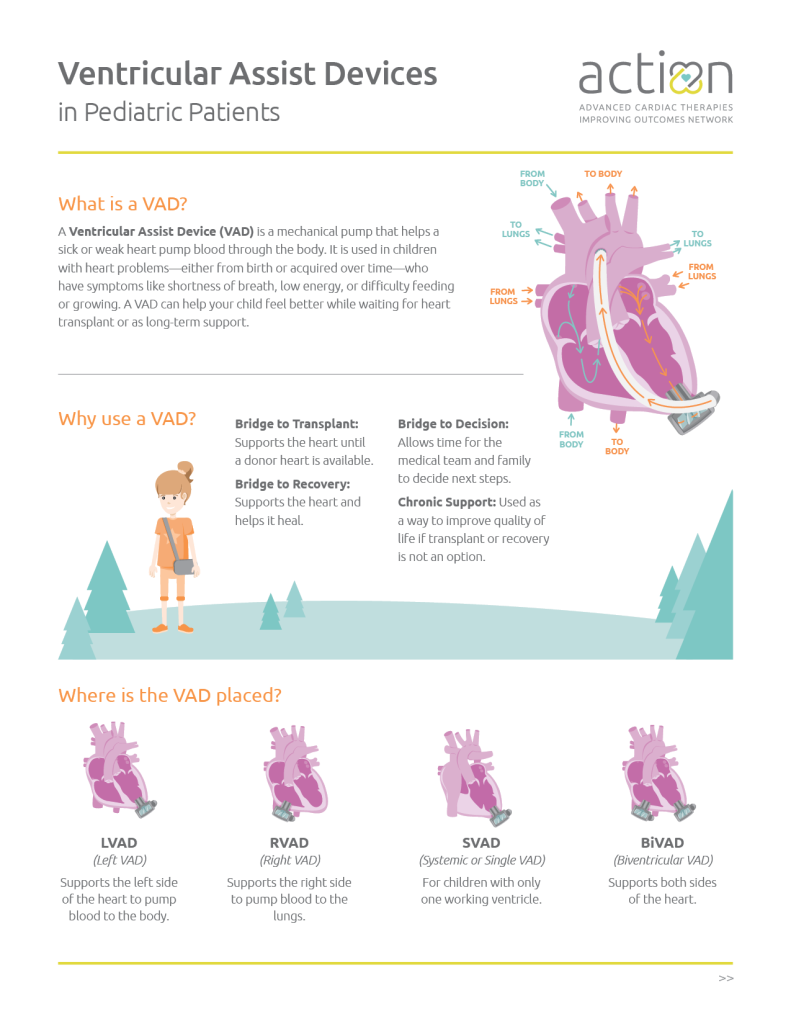
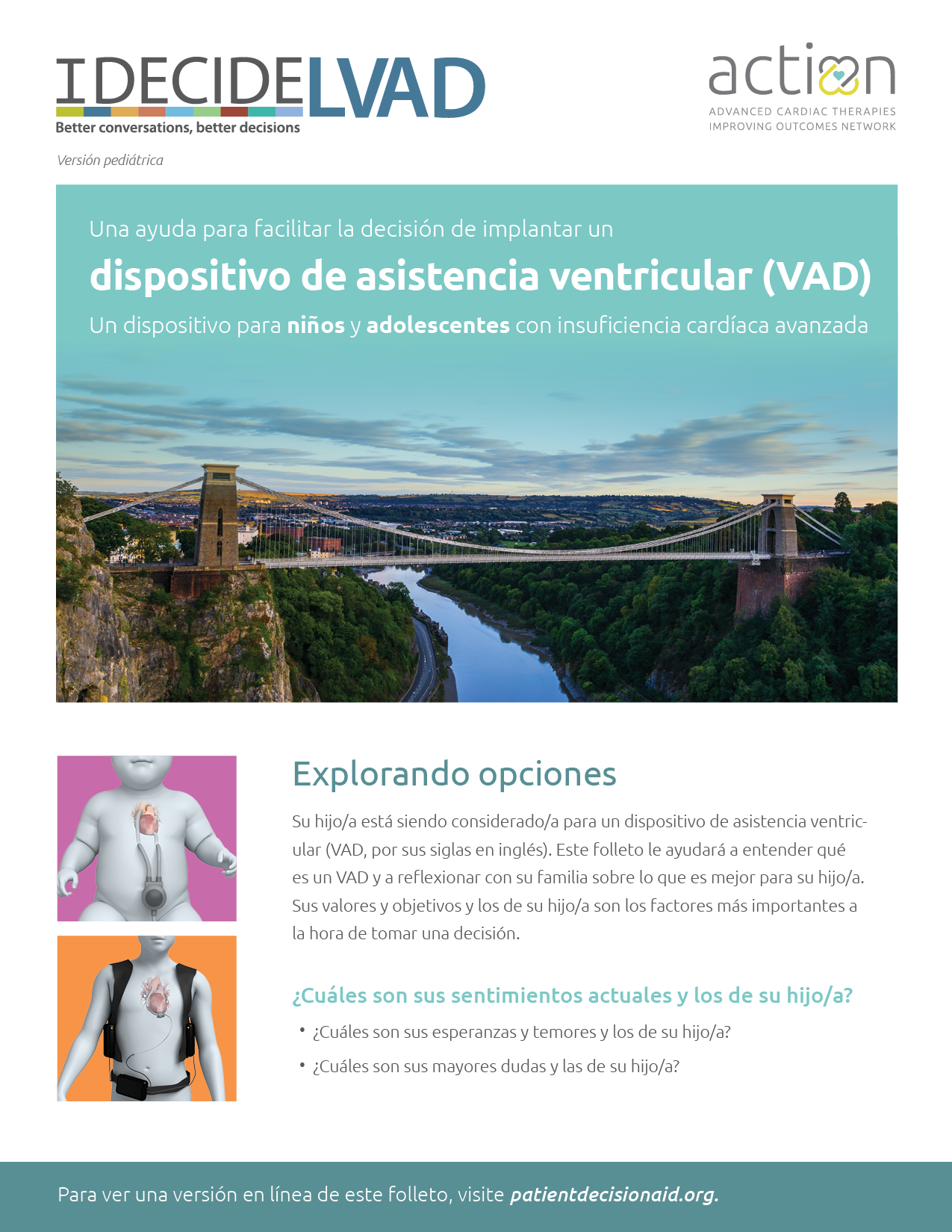
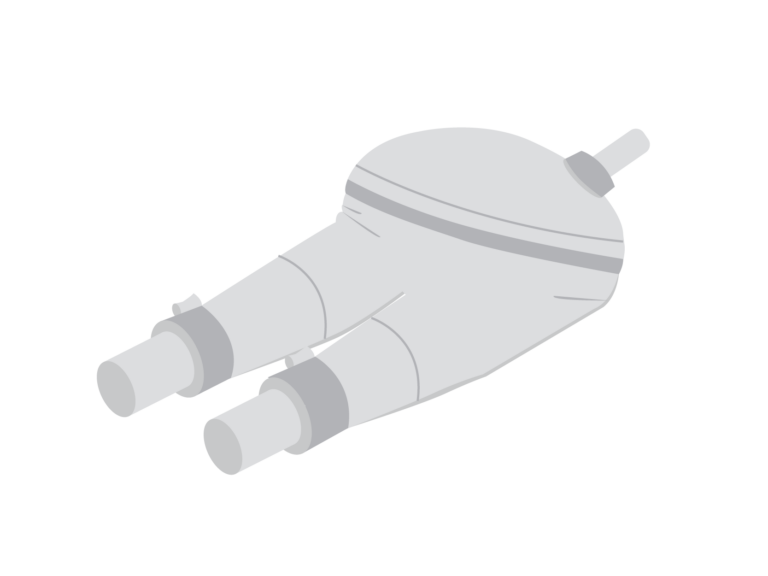
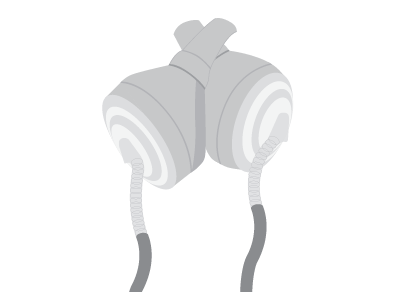
VAD stands for “Ventricular Assist Device.” A VAD is a pump surgically placed in a sick or weak heart to help deliver blood to the body. Children may need a VAD because they are born with a heart problem or because one develops over time. Children with heart failure often have symptoms like feeling short of breath, having trouble eating or gaining weight, and having low energy. A VAD may help these symptoms get better. Sometimes a VAD, depending on the type, will help you feel well enough to leave the hospital and return to school or work. This brief overview explains what a VAD is, why you (or your child) might need one, and what to expect. It helps you quickly understand VAD types, how they support the heart, and possible complications. Let’s take a look at your care journey with a VAD. There are many people that will care for you during your VAD journey, but your care team will guide you throughout the entire journey and always help you make decisions about your care. Just remember, you and your caregivers are a very important part of the team. Your care team may include: VADs can be implanted in any chamber of the heart, but usually they’re located in the left ventricle. The location of the device determines what your VAD may be called. A VAD may be used to help a heart pump for many reasons. Depending on your situation, a VAD may be used as a: Although rare, complications may occur while living with a VAD, which may include: Reducing VAD Risks Hearts & Minds: Neurodevelopment in Patients with Heart Failure & VADs A VAD may be used to help a heart pump for many reasons. Depending on your situation, a VAD may be used as a: Although rare, complications may occur while living with a VAD, which may include: Reducing VAD Risks VADs can be defined by the action that they perform. VADs can pump blood by a spinning action (continuous flow VAD) or by a pumping action (pulsatile flow VAD). Check out this pediatric version of the IDecide VAD decision aid booklet. This booklet was designed for pediatric patients and their families to help them better understand VADs and determine which one might be best for their unique situation. Available in both English and Spanish. Pulsatile flow VADs work by pumping blood in and out of a chamber. Air moves a membrane to fill and eject blood from the chambers to the body. The pump is connected to a large machine called a driver. If you have a pulsatile flow VAD, you will have a pulse. Below are common examples of pulsatile flow VADs. Learn about the Berlin Heart EXCOR®,
how it works, the benefits and risks,
and all about the surgery journey. Learn about the SynCardia Total Artificial Heart (TAH-t), how it works, the benefits and risks, and all about the surgery journey. Continuous flow (CF) VADs work by continuously spinning blood from the weak part of the heart, through the device, out to the aorta, and the rest of the body. There is a small motor located inside the VAD that helps with this spinning motion. The pump is always connected to a controller and requires a power source to keep the VAD spinning. Because the continuous flow device bypasses the weakened heart chamber, you may not be able to feel your pulse. Below are common examples of continuous flow VADs. Learn more about the HeartMate 3™ Learn about the PediMag™ and CentriMag™
Overview
Types
What Are VADs?
The Care Journey
Meet the Care Team


Where is the VAD Implanted?
Benefits
Risks
Benefits

Risks

Although the complications above sound scary, there are many steps you and your care team will take to reduce the possibility of complications. VAD patients will:Resources
See Health & Wellness > Life Style > Resources

Although the complications above sound scary, there are many steps you and your care team will take to reduce the possibility of complications. VAD patients will:
Types of VADs
VAD Decision Aid Booklet
Pulsatile
Berlin Heart EXCOR®
SynCardia (TAH-t)
Continuous Flow
HeartMate 3™ LVAD
LVAD, how it works, the benefits and risks,
and all about the surgery journey.PediMag™
& CentriMag™
VADs, how they work, the benefits and risks,
and all about the surgery journey.
Being on the heart transplant waitlist is a time to be hopeful about the next phase in your journey. There is also a lot to know. Let’s take a few minutes to watch the video below and learn more about the transplant waiting list process. Families and patients sometimes have to wait years for a heart transplant. ACTION is working to help patients become stronger and healthier while they wait for a life-saving transplant. This work has especially touched the hearts of the McQueen Family and they now help lead our efforts! Watch the video below to learn more. For information about transplants, including a patient and family guidebook please visit their website here. Check out our quick facts guide which includes information about: How long could a transplanted heart last?Overview
Waiting for My New Heart
Additional Resources
Pediatric Heart Transplant Society
10 Things for VAD Patients To Know About Pediatric Heart Transplants
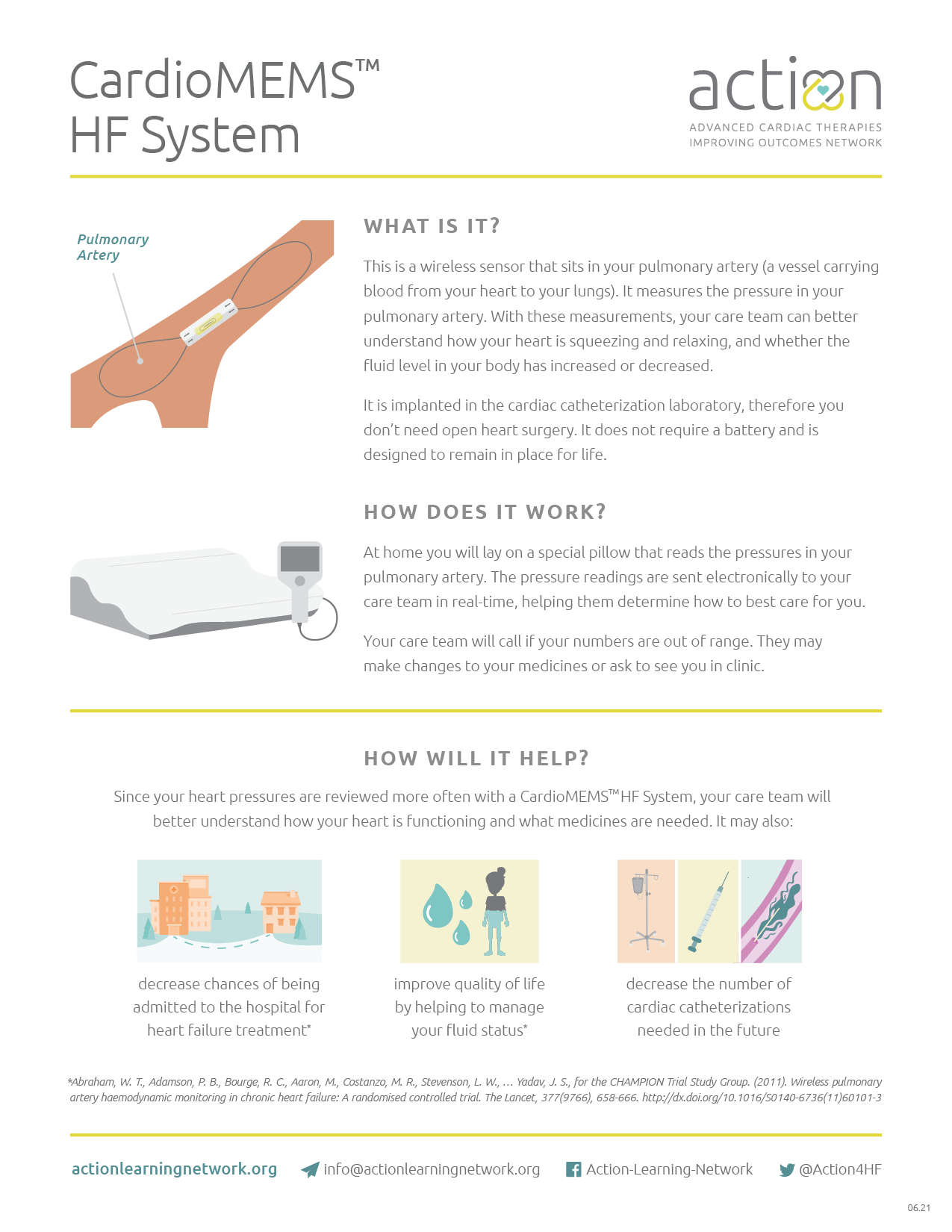
At home you will lay on a special pillow that reads the pressures in your pulmonary artery and sends the readings to your care team electronically. These pressure readings help your care team manage your heart failure symptoms and check for early signs of worsening heart failure. Your care team will call you if your pressure numbers are outside of the range they would like for you. They may need to make changes to your medicines or they may want to see you in person. Want more information? The device is implanted during a cardiac catheterization procedure. Placement does not require an open heart surgery. It has no battery and is designed to remain in place for life. CardioMEMS™ has helped decrease heart failure hospital admissions by almost 50% in adult patients, so it has the potential to decrease your chance of entering the hospital for heart failure treatment. It helps your care team know how the heart is functioning and what medications are needed. CardioMEMS™ can improve your quality of life by: Since your heart pressures are reviewed more often with this device, it may also decrease the need for future cardiac catheterizations. Adverse rates are minimal for CardioMEMS™ placement. The CardioMEMS™ is placed during a cardiac catheterization, so your care team will monitor your insertion site for any bleeding, swelling, or change in color or temperature of your legs. In rare instances, a small blood clot could form at your insertion site and your legs may not get the normal full blood supply to your toes. If this happens, you may have to come back to the hospital for treatment. You will need to be on a blood thinner medicine after the placement of your CardioMEMS™ for a short period of time. This will decrease the risk of additional complications not related to blood clots. CardioMEMS™ has helped decrease heart failure hospital admissions by almost 50% in adult patients, so it has the potential to decrease your chance of entering the hospital for heart failure treatment. It helps your care team know how the heart is functioning and what medications are needed. CardioMEMS™ can improve your quality of life by: Since your heart pressures are reviewed more often with this device, it may also decrease the need for future cardiac catheterizations. Adverse rates are minimal for CardioMEMS™ placement. The CardioMEMS™ is placed during a cardiac catheterization, so your care team will monitor your insertion site for any bleeding, swelling, or change in color or temperature of your legs. In rare instances, a small blood clot could form at your insertion site and your legs may not get the normal full blood supply to your toes. If this happens, you may have to come back to the hospital for treatment. You will need to be on a blood thinner medicine after the placement of your CardioMEMS™ for a short period of time. This will decrease the risk of additional complications not related to blood clots.Overview
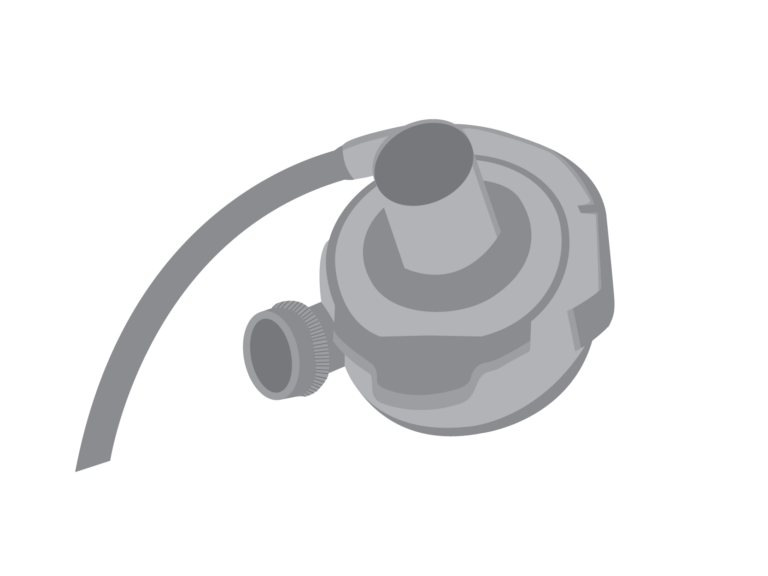
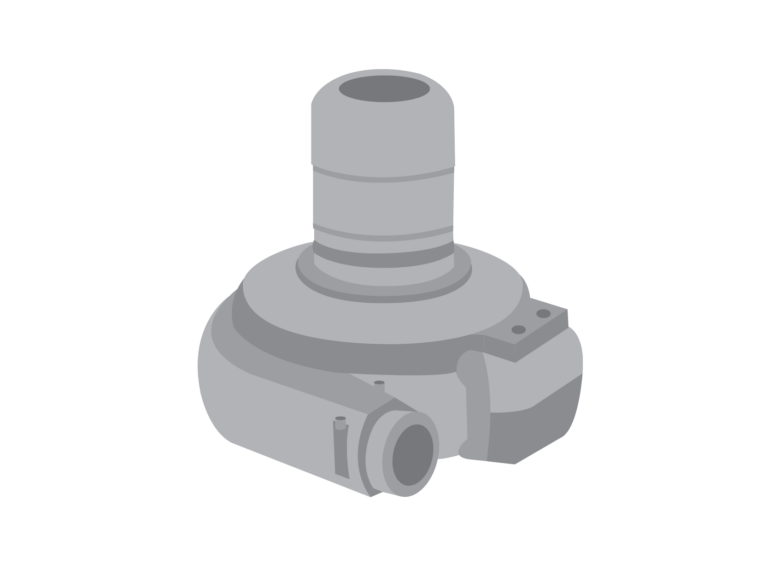
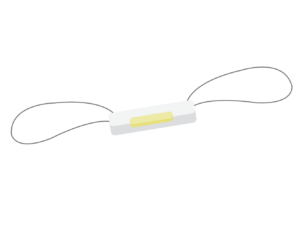 A CardioMEMS™ is an implantable wireless device that sits in the pulmonary artery, a blood vessel that takes blood from your heart to your lungs. The device measures the pressure in your pulmonary artery. The pressure in your pulmonary artery reflects how your heart is squeezing and relaxing, as well as marks how much fluid you have in your body.
A CardioMEMS™ is an implantable wireless device that sits in the pulmonary artery, a blood vessel that takes blood from your heart to your lungs. The device measures the pressure in your pulmonary artery. The pressure in your pulmonary artery reflects how your heart is squeezing and relaxing, as well as marks how much fluid you have in your body.
Check out our CardioMEMs™ HF System patient and family education flyer.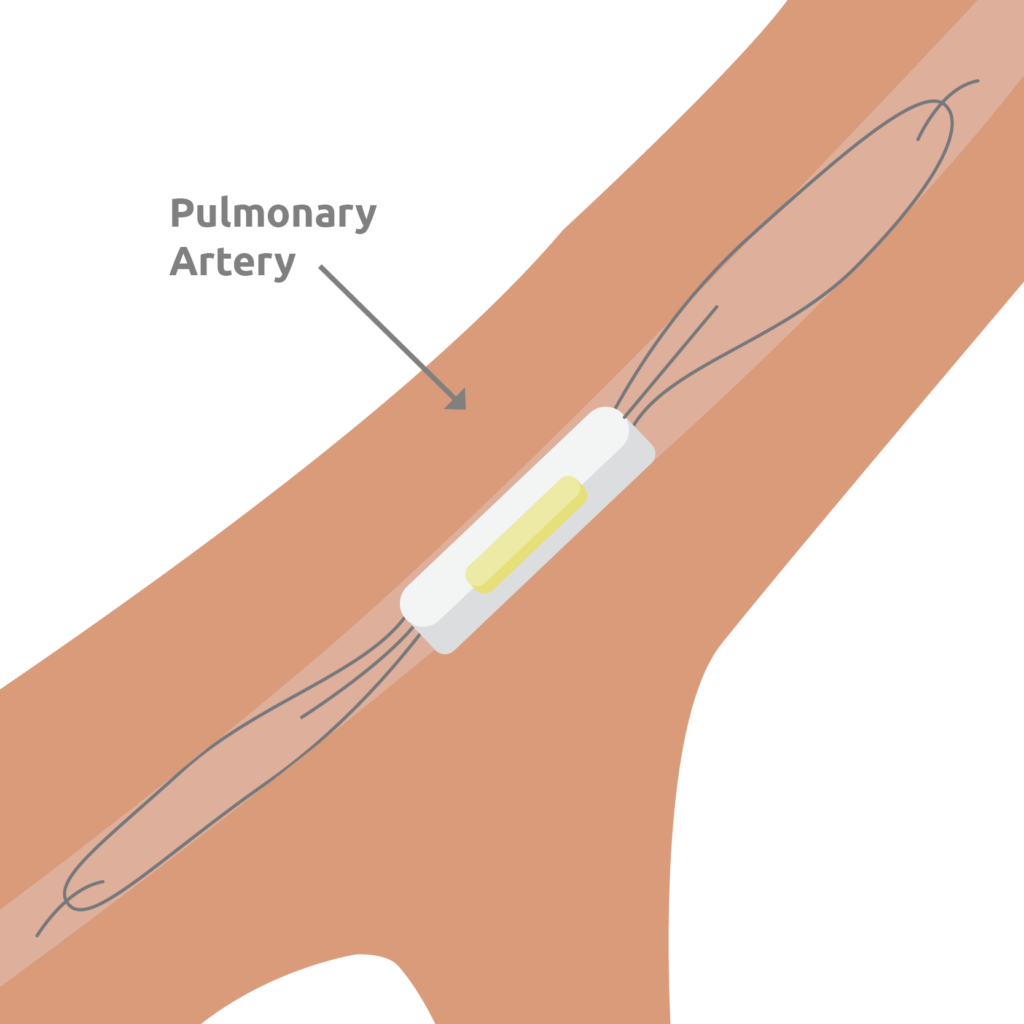
Implanting Your Device
Benefits
Risks
Benefits

Risks